Utilization Patterns of Anticoagulants at Medical Ward of Hiwot Fana Specialized University Hospital, Harar, Ethiopia
Citation: Mengistu G, Lemma B, Molla M. Utilization Patterns of Anticoagulants at Medical Ward of Hiwot Fana Specialized University Hospital, Harar, Ethiopia. J Basic Clin Pharma 2017;8:235-238.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Background: Anticoagulants are drugs used to prevent thrombus extension and embolic complications by reducing the rate of fibrin formation. In a hospital setting anticoagulants are mainly used for the different indications; however, both under-anticoagulation and over-anticoagulation may expose the patient to different problems. The objective of this study was to assess the utilization patterns of anticoagulants at medical ward of Hiwot Fana Specialized University Hospital (HFSUH).
Methods: A retrospective study was conducted at Medical Ward of HFSUH from Medical record of patients’ who take anticoagulants from March 30, 2014 to March 30, 2016. The study was conducted from April 1 to May 10, 2016.
Results: A total of 87 patients over a period of 2 years were on anticoagulant and laboratory monitoring done in HFSUH. More females were on anticoagulant and monitoring. The anticoagulants used were unfractionated heparin, low-molecular weight heparins and warfarin. The most common clinical indications for anticoagulant therapy were lower leg deep vein thrombosis (45.98%), followed by pulmonary embolism (22.98%) and stroke (18.39%). Target INR was achieved in 39.1%, desired clinical outcome was achieved in 37.9%, and minor bleeding complications were seen in 11.5%. Conclusion: The results of this study revealed that the most common clinical indications for anticoagulant therapy were lower leg deep vein thrombosis and the most commonly prescribed anticoagulant drugs was warfarin alone or in combination with other anticoagulants.
Keywords
Anticoagulants, utilization patterns, HFSUH
Introduction
Anticoagulants are drugs used to prevent extension of thrombus and embolic complications by reducing the rate of fibrin formation. Thrombi can form in the veins, artery, or intra-cardium and cause complication through local obstruction, distant embolism in the distal microcirculation and consumption of hemostatic material. Anticoagulants do not directly dissolve already formed clot but prevent recurrences and devastating medical complications by allowing the natural fibrinolytic system to precede normally. [1]
The coagulation pathway plays a pivotal role in the formation and progression of both arterial and venous thrombi. Therefore, drugs aimed at inhibiting this pathway are a major stratagem for the development of novel antithrombotic agents. [2] In a hospital setting anticoagulants are mainly used for disease conditions including deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction (MI), unstable angina, rheumatic heart disease, vascular surgery, prosthetic heart valve, retinal vessel thrombosis, extra corpuscular circulation, hemodialysis and fibrination syndrome. [3]
However, there are two major issues associated with its use: one that is related to under-anticoagulation with attendant clinical thromboembolism and the other over-anticoagulation with complications, particularly bleeding. The use of anticoagulants must follow recommended guidelines; otherwise, it is fraught with increased morbidity and mortality. When anticoagulation is used appropriately, it is an effective and safe practice. [4] This study was aimed to assess the utilization pattern of anticoagulants at the medical ward of Hiwot Fana specialized University Hospital (HFSUH).
Methods
Study setting and period
The study was conducted at medical ward of HFSUH, Harar, Ethiopia. The medical ward has female and male wing and intensive care unit. The study period was from April 1st to May 10th, 2016.
Study design
A hospital based retrospective study was used to assess utilization patterns of anticoagulants by using patient medical record cards.
Populations
The source populations of the study were patient medical record cards found in HFSUH and the study populations were patient medical record cards from March 30, 2014 to March 30, 2016 which contain anticoagulants. Selection criteria: medical record cards of patients received anticoagulants were included in the study and incomplete medical record cards were excluded from the study.
Sampling technique and sample size
Since only 87 patient medical cards were fulfilled the inclusion criteria, all cards were included in the study.
Study variables
Socio-demographic characteristics, co-morbidty, concomitant drug, dosage regimen and duration of anticoagulant therapy were the independent variables and drug interaction, complications, INR/aPTT values and indication of the anticoagulant were dependent variables.
Data collection
Data were collected from patients’ medical record card by using pretested data collection abstraction format by two graduating pharmacy students having basic knowledge of research methodology, pharmacology and pharmacotherapy.
Data quality control
Pre testing of the data collection format was undertaken at surgical ward of HFSUH before the actual data collection and completeness of collected data was checked each time.
Data analysis
The collected data was clean and checked for its completeness, categorized, and analyzed using SPSS version 16.0 software then the result was presented using tables and charts.
Ethical consideration
Before beginning data collection, official permission letter was obtained from school of pharmacy, Haramaya University. Then the letter was submitted to hospital administrative and all the responsible officials are informed about purpose and aim of the study and permission was obtained. After getting consent from the responsible bodies, patients chart were accessed using their card numbers and the confidentiality of data collected was maintained. Name and address of the patient and prescriber is omitted from the data collection format.
Results
Socio-demographic characteristics
In the two year period (2014-2016) only ninety three patients were taking anticoagulant therapy and from these the medical records of six patients were excluded from the study due to incompleteness of the required data and eighty seven medical records were assessed. From these 54.0% were females and most of them (53%) were in the age group of 26-50 years [Table 1].
| Age (years) | Sex | Number (%) |
|---|---|---|
| 15-25 | Female Male |
15 (17.24) 13 (14.94) |
| 26-50 | Female Male |
28 (32.2) 18 (20.69) |
| 51-75 | Female Male |
3 (3.45) 9 (10.34) |
| 76-100 | Female | 1 (1.15) |
| Total | 87 (100) |
Table 1: Socio-demographic characteristic of patient who received anticoagulant therapy at medical wards of HFSU Hospital, from March 30, 2014 to March 30, 2016, Harar, Ethiopia.
Clinical characteristics of the patients and distribution of anticoagulant drug therapy
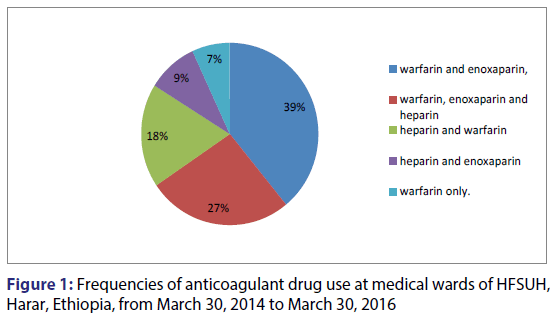
In this study, the most common clinical indications for anticoagulant therapy were lower leg DVT (45.9%) and PE (22.9%). Seventy two patients had co morbidities and the most common co morbid disease was anemia (13%) [Table 2]. During their hospital stay most patients were treated by warfarin and enoxaparin in combination (39.1%) followed by warfarin, enoxaparin and heparin together (26.4%) as shown in Figure 1.
| Clinical characteristics | Number (%) | |
|---|---|---|
| Indication of anticoagulant therapy | Lower leg DVT | 40 (45.98) |
| Pulmonary Embolism | 20 (22.98) | |
| Stroke | 16 (18.39) | |
| Congestive Heart failure, secondary to MVHD, VHD, AF, PE | 8 (9.20) | |
| DVT plus 1st TMP, 3rd TMP | 3 (3.45) | |
| Co-Morbidity | Yes | 72 (82.72) |
| No | 15 (17.24) | |
| Co-morbid disease | Anemia | 13 (13.13) |
| Epilepsy | 11 (11.11) | |
| Diabetes Mellitus | 10 (10.10) | |
| Myocardial infarction | 9 (9.09) | |
| Cellulites | 8 (8.08) | |
| UTI | 7 (7.07) | |
| HIV | 7 (7.07) | |
| Congestive Heart Failure | 7 (7.07) | |
| Tuberculosis | 6 (6.06) | |
| Community acquired pneumonia | 6 (6.06) | |
| Hypertension | 4 (4.04) | |
| Others | 11 (11.11) | |
DVT - Deep Vein Thrombosis; HIV - Human Immune Virus; AF - Atrial Fibrillation; VHD - Valvular Heart Disease; MVHD - Mitral Valve Heart Disease; PE - Pulmonary Embolism, TMP – Trimester of Pregnancy, UTI – Urinary Tract Infection
Table 2: Clinical characteristic of patients on anticoagulant therapy in medical ward of HFSUH from March 30, 2014 to March 30, 2016
Duration of anticoagulant therapy
The duration of therapy of the study patients on anticoagulant were 26(55.32%) of them were on heparin for 5-10 days. On the other hand, the duration of therapies on warfarin greater than 30 days were 46(58.23%). In the case of enoxaparin 43(66.15%) patients had less than 5 days duration of therapy [Table 3].
| Anti-coagulant | Duration of treatment | Number (%) |
|---|---|---|
| Heparin | <5 days | 21 (44.68) |
| 5-10 days | 26 (55.32) | |
| Warfarin | less than 5 days | 7 (8.86) |
| 5-10 days | 4 (5.06) | |
| 10-30 days | 22 (27.85) | |
| greater than 30 days | 46 (58.23) | |
| Enoxaparin | less than 5 days | 43 (66.15) |
| 5-10 days | 22 (33.85) |
Note: the duration of therapy given above includes bridge therapies like heparin and warfarin and enoxaparin.
Table 3: Duration of anticoagulant therapy at medical wards of HFSUH, Harar, Ethiopia from March 30, 2014 to March 30, 2016
Drugs co-administered with warfarin and their potential drug interaction with warfarin
A total of 236 drugs were prescribed with warfarin and from these Injectable anticoagulants (20.8%) were the most common [Table 4]. Out of 236 drugs co-administer with warfarin, 140 drugs have a potential drug-drug interaction with warfarin and the most common drug was unfractionated heparin (35%) followed by enoxaparin and aspirin both accounts 10.7% [Table 5].
| Class of drugs | Administered drugs | Number (%) |
|---|---|---|
| Antibiotics | Cloxacillin 500 mg I.V. QID Ceftriaxone 1 g I.V. BID Augmentin 625 mg P.O.TID Metronidazole 500 mg I.V TID B.pencilline 1.2 million IU Ciprofloxacin 500 mg, P.O. BID Norfloxacin 400 mg P.O. BID Azithromycin P.O. 500 mg QD Cephalexin P.O 500 mg B.I.D |
8 (3.39) 14 (5.93) 3 (1.27) 4 (1.69) 3 (1.27) 8 (3.39) 5 (2.12) 6 (2.54) 6 (2.54) |
| Non-Steroidal Anti-inflammatory Drugs | Diclofenac 75 mg IM Injection Aspirin 81 mg PO QD Tramadol 100 mg IM |
10 (4.24) 15 (6.35) 5 (2.12) |
| Injectable anticoagulants | UFH 5000 IU iv stat, SC Enoxaparin 60 mg SC bid |
49 (20.76) 15 (6.35) |
| Diuretics | Hydrochlorothiazide 25 mg P.O.Q.D Furosemide 40 mg P.O. daily Furosemide 40 mg iv |
10 (4.24) 4 (1.69) 8 (3.39) |
| Cardiovascular | Digoxin 0.25 mg Atenolol 50 mg P.O. Q.D Enalapril 2.5 mg P.O B.I.D |
7 (2.97) 5 (2.12) 4 (1.69) |
| Anti-tuberculosis | 2EHRZ (400, 150, 75, 400) mg | 6 (2.54) |
| Anti-diabetic | Metformin 500 mg P.O. B.I.D | 10 (4.24) |
| Anti-Retroviral drugs | TDF, 3TC, EFV (300, 300, 600) mg | 7 (2.97) |
| Antiepileptic Drugs | Phenobarbital 100 mg | 11 (4.66) |
| Iron product | Ferrous Salts PO 200 mg TID | 13 (5.51) |
| Total | 236 | |
UFH - Unfractionated Heparin; EHRZ - Ethambutol, Isoniazid Pyrazinamide and Rifampicin, Anti-Retroviral (ART), Tenofovir, Lamivudine and Efavirenz (TDF, 3TC, EFV)
Table 4: Drugs that are co-administered with warfarin in HFSUH at MW from March 30, 2014 to March 30, 2016
| Potentially Interacting drugs | Frequency | Percentage (%) |
|---|---|---|
| UFH 17,500 IU S.C BID | 49 | 35 |
| LMWHs (enoxaparin) 60 mg S.C TID | 15 | 10.71 |
| Aspirin 81 mg P.O. daily | 15 | 10.71 |
| Ceftriaxone 1 g I.V. BID | 14 | 10 |
| Phenobarbital 100 mg | 11 | 7.87 |
| Diclofenac 75 mg I.M. Injection | 10 | 7.14 |
| Ciprofloxacin 500 mg, P.O. BID | 8 | 5.71 |
| Rifampicin (anti Tb) | 6 | 4.29 |
| Tramadol 100 mg I.M Injection | 5 | 3.57 |
| Metronidazole 500 mg iv TID | 4 | 2.86 |
| Augmentin 625 mg P.O. TID | 3 | 2.14 |
| Total | 140 | 100% |
Table 5: Drugs that have potential drug-drug interaction with warfarin in HFSUH at medical ward from March 30, 2014 to March 30, 2016
Coagulation profiles of study participants
All study participants had coagulation profile such as INR and aPTT and these tests were repeated during their stay in the hospital in order to monitor the efficacy of the anticoagulant therapy. As recorded on the medical records 252 INRs and 239 aPTT tests were performed. Among the INR values only 39.28% were within the therapeutic range and most of aPTT values (36.8%) were less than ≤ 26 [Table 6].
| Coagulation profile | Frequency | Percent (%) | |
|---|---|---|---|
| INR range | ≤ 1.2 | 33 | 13.09 |
| 1.2-1.5 | 39 | 15.47 | |
| 1.5-2.0 | 49 | 19.45 | |
| 2.0-3.0 | 99 | 39.28 | |
| 3.0-4.5 | 22 | 8.72 | |
| 4.5-9.0 | 7 | 2.78 | |
| 9.0-10.0 | 3 | 1.19 | |
| aPTT Range | ≤ 26 | 88 | 36.82 |
| 26-30 | 63 | 26.36 | |
| 30-40 | 38 | 15.89 | |
| 40-50 | 34 | 14.24 | |
| 50-100 | 8 | 3.35 | |
| ≥ 100 | 8 | 3.35 | |
| INR values | Below therapeutic range | 121 | 48.01 |
| Within therapeutic range | 99 | 39.28 | |
| Above therapeutic range | 32 | 12.69 | |
Note: aPTT: Activated partial Prothrombin time, INR: International Normalized Ration, INR range (0.73-9.2), aPTT range (14.5-153)
Table 6: Number of study participants on laboratory monitoring at medical wards of HFSUH from March 30, 2014 to March 30, 2016, Harar, Ethiopia.
Clinical outcome and complication of anticoagulant therapy
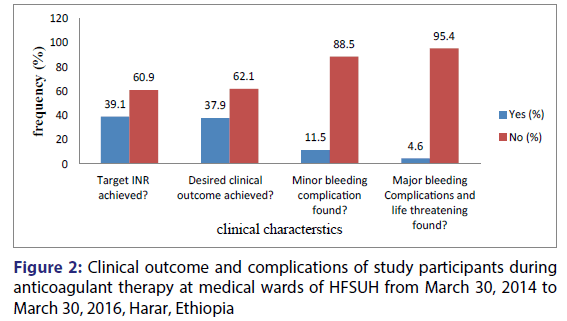
In this study target INR was achieved in 39.09% of the study participants and desired clinical outcome was achieved in 37.93% study participants. Minor bleeding complications as gingival and genitourinary bleedings were seen in 11.6% of study participants and major bleeding and life threatening as GI bleedings and incidental nasal bleeding were reported in 4.6% of the study participants [Figure 2].
Discussion
The present study was aimed to assess the utilization patterns of anticoagulants at medical ward of HFSUH. In this study, the most common indications of anticoagulant therapy were lower leg DVT (45.98%) and PE (22.98%). Similarly studies from Nigeria and Kenya also reported the major indication for anticoagulants were DVT and PE. [5,6] But a population-based retrospective cohort study in Minnesota, USA showed that the major indications for anticoagulants were VTE (39%) and transient ischemic attack (21%). [7] The presence of more DVT indications in this study might be correlated with the incidence of thromboembolic complications. The achievement of desired anticoagulation is low in Africa, ranging from 7% to 30% in Kenya (40); 39% in Nigeria [6] and 32-58% in South Africa [8] which is comparable to the result of this study (39.1%). Reaching optimal target in anticoagulation is directly related to the infrastructure of anticoagulation services available. Studies from USA, China and Canada showed a higher level of achievement of desired anticoagulation compared to data from African centers. [4]
This study also revealed that 82.7% of the study participants had a co morbid condition and the most common co morbid disease was anemia. The most commonly used anticoagulant used in this study were warfarin and enoxaparin in combination and around 91% of the study participant used warfarin alone or in combination with other anticoagulants. Since most patients had a co morbid condition they used additional drugs to treat the co morbidities and the most commonly drugs concomitantly used with warfarin were Injectable anticoagulants. These drugs had a potential to interact with warfarin and might lead to bleeding which is a cause of anemia (most common co morbid condition in this study).
In the present study, the incidence of bleeding complications was 16.1% which is comparable with study done by Wehinger et al. which was 14.6%. [9] Another study done in USA [7] showed the three months cumulative incidence of bleeding were 20.8%. Different researches show a difference in risk of bleeding complication which might be due to difference in the set-up, drugs used and other factors.
The incidence of complication may be related with the presence of concomitant drugs, the use of more than one anticoagulant and co morbid conditions but in this study none of them showed significant association with bleeding. Desired clinical outcome and adequate dosing was achieved only in 37.93% of the patients [Table 6]. Anticoagulation service in HFSUH is still evolving, and there are challenges associated with it. There is a need for dedicated anticoagulation services with defined roles and mission.
Conclusion
The present study revealed that the most common clinical indications for anticoagulant therapy were lower leg deep vein thrombosis and the most commonly prescribed anticoagulant drugs was warfarin alone or in combination with other drugs. Above half of the co-administered drugs had potential drug interaction with warfarin. The most INR values were not in the therapeutic range and this may lead to low desired clinical outcome. The inappropriate utilization patterns of anticoagulants may also compromise patient safety.
Conflict of interest
The authors declare that there is no conflict of interest
Acknowledgements
We would like to thank School of pharmacy, Haramaya University for provision of material supports. We also extend our deepest gratitude and appreciation for HFSUH staffs and our data collectors for their kindly support during data collection.
REFERENCES
- Singh V, Gopinath K, Behzadpour A, Meera NK. Anticoagulant Utilization Evaluation in a Tertiary Care Teaching Hospital, An Observational Prospective Study in Medical in Patients. Indian Journal of Pharmacy Practice 2015;8:61-6.
- Khoo CW, Tay KH, Shantsila E, Lip G. Novel oral anticoagulants.International Journal of Clinical Practice 2009;63:630-41.
- Geerts WH, Pineo GF, Heit JA. Prevention of venous thrombo embolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004;126:338-400.
- Bauer KA. New anticoagulants. Curr Opin Hematol 2008;15:509-15.
- Anakwue RC, Ocheni S, Madu AJ. Utilization of oral anticoagulation in a teaching hospital in Nigeria. Annals of Medicine and Health Sciences Research 2014;4:286-90.
- Pastakia SD, Crisp WI, Schellhase EM, Manji I, Ouma MN, Akwanalo C. Implementation of a pharmacist managed anticoagulation clinic in Eldoret, Kenya. Southern Med Review 2010;3:20-3.
- Gitter MJ, Jaeger TM, Petterson TM, Gersh BJ, Silverstein MD.Bleeding and thromboembolism during anticoagulant therapy, a population-based study in Rochester, Minnesota. Mayo Clin Proc 1995;70:725-33.
- Tiryaki F, Nutescu EA, Hennenfent JA, Karageanes AM, Koesterer LJ, Lambert BL, et al. Anticoagulation therapy for hospitalized patients patterns of use, compliance with national guidelines and performance on quality measures. Am J Health Syst Pharm 2011;68:1239-44.
- Wehinger C, Stöllberger C, Länger T, Ing D, Schneider B, Finsterer J. Evaluation of risk factors for stroke/embolism and of complications due to anticoagulant therapy in atrial fibrillation. Stroke 2002;32:2246-52.