Use and Safety of Valproic Acid for Patients with Behavioural and Psychological Symptoms in a Cognitive Behavioural Unit: Retrospective Study
2 Institut National de la santé et de la Recherche Médicale INSERM (French National Health and Medical Research Institute), Institut des Maladies Mét, Unit 1048, Team 6: Cardiac Remodelling and New Therapies, INSERM, I2MC, 1 avenue du Professeur Jean Poulhès, France
3 Institut National de la Santé et de la Recherche Médicale INSERM, Unit 1027 Team 1: Ageing and Alzheimer’s Disease: From Observation to Intervention. INSERM U1027, 37 Allées Jules Guesde, France
4 Pharmaceutical Sciences, University of Toulouse, Toulouse III, Clinical Pharmacy Department, 35 Chemin des Maraîchers, France
5 University Hospital, Toulouse, Geriatrics Department, 170, Avenue de Casselardit TSA 40031, France
6 University Hospital, Toulouse, Psychiatric Department, 330 Avenue de Grande Bretagne, France
7 Institut National de la Santé et de la Recherche Médicale INSERM, Toulouse Neuroimaging Center ToNIC UMR1214 - Inserm/UPS, CHU PURPAN - Pavillon BAUDOT Porte 305, 31024, Toulouse CEDEX 3, France
Citation: Rouzaud Laborde C, Rouch L, Rigal A, Sallerin B, Voisin T, Arbus C, Cestac C. Use and Safety of Valproic Acid for Patients with Behavioural and Psychological Symptoms in a Cognitive Behavioural Unit: Retrospective Study. J Basic Clin Pharma 2018;9:04-08.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Introduction: The management of behavioural disorders in the elderly is a reality that is difficult to implement. Few studies have focused on the therapeutic arsenal for managing these numerous conditions which will only increase in the years to come, in view of our ageing population. In cases where medical and non-medical strategies fail, valproic acid could provide an alternative based on studies that have highlighted its effects in the management of behavioural disorders. However, VA can cause sedation due to excessive ammonia levels in the blood, which may prove toxic for the central nervous system. The purpose of this study was to monitor any beneficial effects of VA in the treatment of behavioural disorders in a cognitive-behavioural unit (CBU), to measure ammonia levels in the blood after initiating treatment and, finally, to study combinations of psychotropic treatments with and without VA on patients’ discharge prescriptions. Patients and Methods: This retrospective study was carried out in a 13-bed cognitive behavioural unit over an 18-month period from November 2011 to May 2013. All of the patients who had received VA on at least one occasion were enrolled in the study. Ammonia levels in the blood were assayed by nursing staff. The clinical course was documented in the medical records and NPI scores (on admission and discharge) were collected. Finally, the discharge prescriptions issued by the CBU were analysed. Statistical tests were carried out using Graph Pad Prism 6. Results: Out of 35 patients with an average age of 80 +/-1 year, who received VA, 20 (57%) discharged from the CBU with this treatment benefited from it. The levels of ammonia recorded in the blood of these patients did not differ from those of patients who either did not respond or responded unfavourably to VA (treatment discontinued), namely 53.29 +/-4.7 mg/L and 63.50+/-6.7 mg/L (p=0.21), respectively. Blood ammonia levels do not appear to be implicated in the favourable clinical course of patients receiving VA. Finally, the inclusion of VA in discharge prescriptions allows a significant saving to be made in terms of neuroleptic agents (p=0.0017) and benzodiazepines (p= 0.0006), which are known to be iatrogenic in the elderly. Conclusion: valproic acid proved to be beneficial for 1 in 2 patients admitted to a cognitive behavioural unit since the discharge prescriptions contain this medicinal product. In fact, these results are consistent with doctors’ medical observations. However, the statistics quoted by the NPI do not highlight the effect of valproic acid. When included in discharge prescriptions, VA promotes savings in terms of psychotropic medication.
Keywords
Behavioural disorder; valproic acid; blood ammonia levelsIntroduction
The management of elderly hospitalised patients is a real concern for medical and nursing staff. Apart from the fact that the patients are often receiving multiple medication, they present with several concomitant diseases which complicates the overall treatment process. They are often fragile and maintaining their independence must remain a priority. [1] The somatic treatment of elderly patients can be compounded by behavioural problems. The latter are very often associated with neurodegenerative, vascular or combined forms of dementia in this patient population.[2] The management of these patients sometimes calls for specialist facilities known as cognitive behavioural units (CBU), which mainly use non-pharmacological methods although a pharmacological approach can also be adopted, as required, in terms of overall patient management.[3] This type of management strategy will develop even further in the foreseeable future, given the ageing of the population. Unfortunately, only a few clinical studies are carried out in the elderly because of a specific, non-interventional culture adopted for this patient cohort. Psychotropic drugs are used when nonpharmacological methods fail within the CBUs. However, the majority of these medicinal products have not been studied in dementia-related behavioural disorders. Furthermore, there is evidence that the class of antipsychotic drugs causes adverse reactions such as drowsiness, urinary problems and extrapyramidal syndrome on the one hand, which alter a patient’s quality of life[4,5] and increases cardiovascular morbi-mortality in the elderly. This has led to considerable restrictions on these drugs in these indications.[6] CBU doctors are sometimes at a disadvantage when it comes to treating behavioural disorders that prove refractory to non-pharmacological methods. Valproic acid is an active substance widely used as a normothymic agent to regulate the mood of bipolar patients by modulating GABAergic and glutamatergic transmissions.[7] When used in the treatment of behavioural disorders, valproic acid has had beneficial effects on bipolar[8], schizophrenic[9] patients but these results remain controversial in adolescents[10] and dementia patients[11] with a concomitant, non-negligible risk.[12] Some authors have also tested valproic acid in the management of dementiarelated behavioural disorders in the elderly but results also remain sketchy and controversial with regard to some clinical symptoms such as agitation, for instance.[13] Valproic acid is known to trigger excessive ammonia levels in the blood. These are serious adverse effects which sometimes envelop the patient in states of drowsiness due to the sedative central effect of ammonium ions that pass through the bloodbrain barrier.[14] The aim of this study was to observe the short- and mid-term efficacy of valproic acid in patients presenting behavioural disorders including aggression, refusal of care, agitation and impulsive behaviour in situations where other medicinal and non-medicinal treatments have proved ineffective. Valproic acid has been assessed in a CBU for the very first time. The study also focused on establishing an optimum patient profile for response to treatment. The efficacy of valproic acid was compared to excessive ammonia levels observed in these patients during their hospital stay and related psychotropic drugs included in the discharge prescriptions.
Patients and Methods
This study was observational and retrospective. It was carried out within a professional practice evaluation framework. No ethics committee was consulted. This study reflects on the care given to patients during their stay in a cognitive behavioural unit. No medical procedure was carried out and no prescription was administered specifically for this study. All of the data are part of the current care package.
Study location and duration
The study was carried out from 28/11/2011 to 24/05/2013 in a 13- bed cognitive behavioural unit (CBU). A hospital neurologist and a psychiatrist practise in this unit. One medical intern and a registrar specialising in neurology were also present. A clinical pharmacist analysed prescriptions on a daily basis.
Inclusions
All patients presenting one or more of the following clinical symptoms were enrolled in the study: opposition, aggression, agitation or impulsive behaviour following the failure of non-medicinal treatment and medication, which may or may not be dementia-related and who had taken valproic acid in the unit on at least one occasion to treat behavioural disorders.
Clinical and laboratory data
The following data were recorded: the patients’ initials, gender, kidney function, history of liver disease or liver failure, prothrombin time and NPI scale on admission and discharge. Ammonia levels in the blood were recorded prior to the introduction of valproic acid and during treatment, if administered. For each patient, the daily medical observations were re-read and favourable clinical courses or clinical improvements were documented. Clinical courses were deemed favourable if the following key words appeared at least once in the medical notes: “improvement” in disorders, “fewer clinical signs” such as aggression, agitation, refusal or impulsive behaviour, “disappearance of disorders”, “efficacy” and “fewer disorders present”. Clinical courses were considered unfavourable if the following words appeared at least once in the medical records: “persistent disorders”, “inefficacy” “not effective”, “lack of efficacy”, “discontinuation of treatment”, “clinical signs of excessive levels of ammonia in the blood”, “persistent clinical signs” such as aggression, agitation, refusal and impulsive behaviour.
Medical prescription data
Valproic acid was introduced at an appropriate dose level for each patient and was increased depending on clinical efficacy, clinical tolerance and individual ammonia levels in the blood. Analyses of prescriptions issued in addition to valproic acid were recorded on the CBU discharge prescriptions. The inclusion or exclusion of neuroleptics, benzodiazepine anxiolytics and antidepressants was noted.
Results
Clinical course (NPI) in patients who received valproicacid during their hospital stay
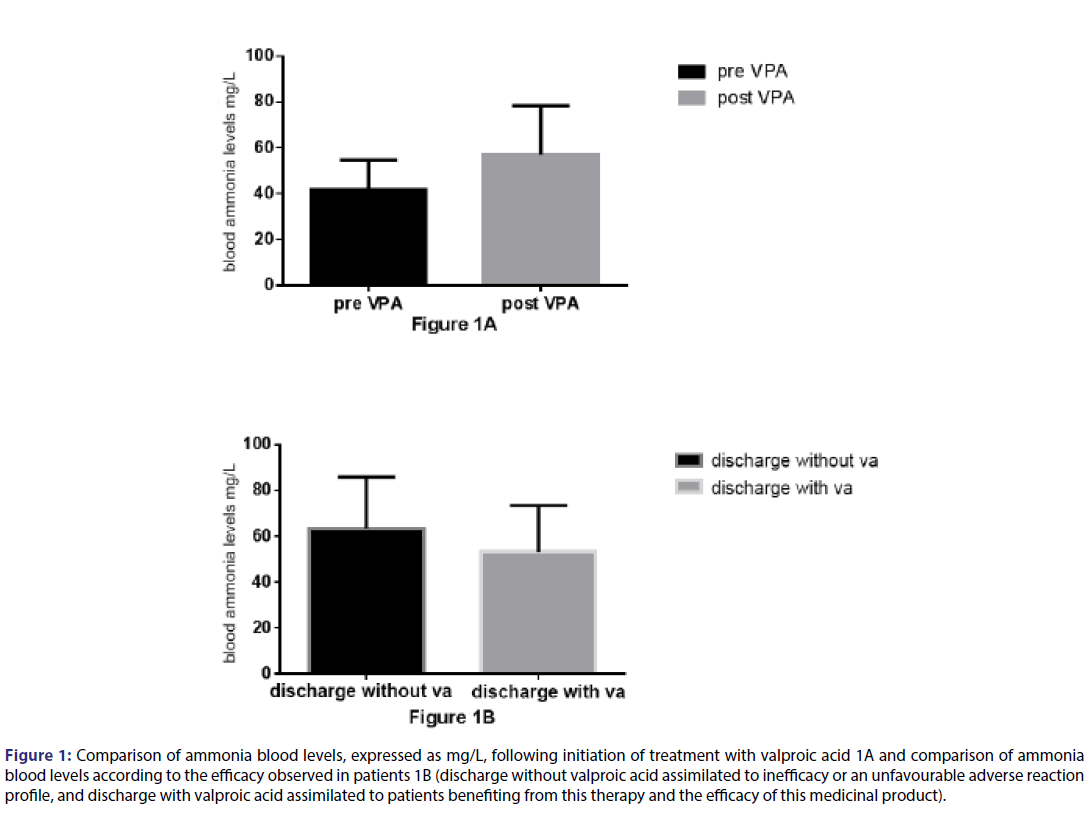
Valproic acid seems to significantly increase ammonia levels in the blood in patients receiving this treatment, with values increasing from 41.97+/- 3.2 mg/L prior to treatment to 57.16 +/- 3.9 mg/L (p=0.015) after treatment had started [Table 1; Figure 1A]. However, patients with a favourable clinical response to valproic acid and discharged with this treatment presented with ammonia levels of 53.29 +/-4.7 mg/L in the blood. This level does not differ significantly from that recorded in patients with no favourable clinical response and who were not discharged with valproic acid [(increase to 63.50+/-6.7 mg/L (p=0.21)]. This level even tends to fall in patients who benefited from treatment [Figure 1B]. Excess ammonia levels in the blood, which manifest in the form of central sedative effects, cannot therefore be responsible for the clinical effects observed in terms of an improvement in behavioural disorders in the patient population discharged with valproic acid.
Figure 1: Comparison of ammonia blood levels, expressed as mg/L, following initiation of treatment with valproic acid 1A and comparison of ammonia blood levels according to the efficacy observed in patients 1B (discharge without valproic acid assimilated to inefficacy or an unfavourable adverse reaction profile, and discharge with valproic acid assimilated to patients benefiting from this therapy and the efficacy of this medicinal product).
| N=35 patients who received valproic acid | |
|---|---|
| Age mean +/- SD (years) | 80+/-1 |
| Male gender n(%) | 23 (66) |
| Creatinine clearance Cockroft and Gault mean +/- SD (ml/min) | 67+/-6 |
| History of liver disease n(%) | 0 (0) |
| Liver failure n(%) | 0 (0) |
| History of epilepsy n(%) | 5 (14.7) |
| Clinical signs evident on admission, recorded in medical observations | |
| Refusal n (% of patients) | 13 (37) |
| Aggression n (% of patients) | 29 (83) |
| Agitation n (% of patients) | 21 (60) |
| Impulsive behaviour n (% of patients) | 9 (26) |
| Neuropsychiatric inventory NPI on admission agitation/aggression Mean +/-SD |
6.24+/-0.85 |
| Neuropsychiatric inventory NPI on admission irritability/mood swings Mean +/-SD |
5.53+/-0.86 |
| Clinical signs evident on discharge | |
| Neuropsychiatric inventory NPI on discharge agitation/aggression Mean +/-SD |
5.35+/-0.70 |
| Neuropsychiatric inventory NPI on discharge irritability /mood swings Mean +/-SD |
4.81+/-0.72 |
| Main procedures – Common Classification of Medical Procedures – during the patient’s stay | |
| Refusal n (% of patients) Aggression n (% of patients) Agitation n (% of patients) Impulsive behaviour n (% of patients) Dementia n (% of patients) Neurodegenerative dementia n (% of patients) Vascular dementia n (% of patients) Non-specified dementia n (% of patients) |
19 (54) 8 (23) 21 (60) 13 (37) 21 (60) 12 (34) 4 (11) 5 (14) |
Table 1: Profile of blood ammonia levels in patients who received valproic acid during their hospital stay
Clinical course (NPI) in patients who received valproic acid during their hospital stay
The efficacy of hospitalisation in a specialist CBU and the medical / non-medical management approaches were studied on the basis of NPI items listed in detail in Table 2. The mean item scores for the patients were calculated on admission and discharge. Two groups were created to shed light on the potential effect of valproic acid on NPI items: patients who responded favourably to VA and discharged from the CBU with VA, and those who did not respond favourably to VA and who were discharged without VA. The mean NPI admission scores versus NPI discharge scores did not differ significantly in the group benefiting from VA and discharged with VA. Conversely, in the group of patients discharged without valproic acid, 2 mean NPI scores differed significantly between patient admission and discharge. These were aberrant motor behaviour (p=0.02) and sleep (p=0.04). Valproic acid does not appear to significantly affect NPI scores in the CBU or else the power of our study is limited in highlighting any difference. A comparison of NPI admission scores between unit patients in the 2 groups (discharged with valproic acid and without valproic acid) highlighted a predictive factor in favour of non-response to valproic acid treatment: sleep. In fact, patients discharged from the CBU without valproic acid had a significantly higher NPI sleep score on admission (mean 4.0+/-1.2) than that recorded in patients discharged from the CBU with valproic acid (0.6+/-0.4; p=0.007) [Table 2], last column. However, these results appear controversial based on an analysis of the daily medical observations in the patients’ records. More patients with valproic acid had at least one favourable clinical course entered in their medical record compared to the number of patients discharged without VA (p=0.007) [Table 3].
| NPI item | Patient discharged with VA Mean +/- SD |
Patient discharged without VA Mean +/- SD |
Patient profile: on admission p |
||||
|---|---|---|---|---|---|---|---|
| Mean NPI score on admission | Mean NPI score on discharge | p | Mean NPI score on admission | Mean NPI score on discharge | p | ||
| Delirious thoughts | 1.4+/-0.8 | 0.3+/-0.2 | 0.41 | 4.1+/-1.5 | 0.9+/-0.7 | 0.07 | 0.07 |
| Hallucination | 0.5+/-0.3 | 0.2+/-0.2 | 0.60 | 2.5+/-1.3 | 0.08+/-0.08 | 0.09 | 0.22 |
| Agitation/ aggression |
5.6+/-1.1 | 5.2+/-0.9 | 0.84 | 7.6+/-1.4 | 5.1+/-1.1 | 0.18 | 0.23 |
| Depression/ dystrophy |
1.1+/-0.7 | 1.0+/-0.7 | 0.93 | 0.2+/-0.2 | 1.0+/-0.7 | 0.48 | 0.45 |
| Anxiety | 4.1+/-1.1 | 3.2+/-1.1 | 0.67 | 3.5+/-1.4 | 2.7+/-1.3 | 0.73 | 0.74 |
| Elation | 0.6+/-0.3 | 0.8+/-0.4 | 0.71 | 0.8+/-0.6 | 0.7+/-0.5 | >0.9 | 0.88 |
| Apathy/ indifference |
2.8+/-1.1 | 2.2+/-0.9 | >0.9 | 1.4+/-0.8 | 2.3+/-1.1 | 0.61 | 0.63 |
| Disinhibition | 2+/-0.8 | 0.8+/-0.5 | 0.28 | 2.2+/-1.2 | 2.3+/-1.1 | >0.9 | 0.87 |
| Irritability/ mood swings |
4.4+/-1.1 | 5.3+/-0.9 | 0.57 | 7.1+/-1.3 | 3.8+/-1.2 | 0.08 | 0.16 |
| Aberrant motor behaviour | 4.0+/-1.2 | 3.8+/-1.1 | 0.98 | 6.8+/-1.2 | 2.6+/-0.8 | 0.02 | 0.12 |
| Sleep | 0 .6+/-0.4 | 0.5+/-0.3 | >0.9 | 4.0+/-1.2 | 0.9+/-0.2 | 0.04 | 0.007 |
| Appetite | 4.6+/-1.1 | 3.2+/-1.0 | 0.36 | 5.1+/-1.4 | 2.3+/-1.1 | 0.16 | 0.79 |
Table 2: The efficacy of hospitalisation in a specialist CBU and the medical /non-medical management approaches were studied on the basis of NPI items
| Favourable observation | Unfavourable observation | Not known | Total | |
|---|---|---|---|---|
| Patient discharged with VA | 13 | 3 | 5 | 21 |
| Patient discharged without VA | 3 | 10 | 4 | 17 |
| Total | 16 | 13 | 9 | 38 |
Table 3: More patients with valproic acid had at least one favourable clinical course entered in their medical record compared to the number of patients discharged without VA
Out of the 35 patients who tested VA, 20 (57%) left the CBU with this treatment and responded favourably, benefiting from this treatment. 15 patients did not experience any benefit from taking VA (43%). A comparison of these 2 patient cohorts in terms of numbers differs with regard to concomitant neuroleptic administration: patients with VA had fewer neuroleptic prescriptions (p=0.0017). The same profile is apparent with concomitant hypnotic and/or anxiolytic benzodiazepine therapy. Fewer patients with VA were prescribed benzodiazepines concomitantly (p=0.0006) [Table 4].
| Discharge prescription type n(%) |
Discharged with VA 20 (57) |
Discharged without VA 15(43) |
p |
|---|---|---|---|
| VA only n(%) | 12 (60) | 0 | NA |
| With neuroleptic n(%) | 2 (10) | 10 (66.6) | 0.0017 |
| With benzodiazepine n(%) | 6 (30) | 14 (93) | 0.0006 |
| With antidepressants n(%) | 2 (10) | 3 (20) | 0.63 |
Table 4: CBU Discharge Prescription Profile for patients who received VA
Discussion and Conclusion
During this study, we were able to highlight the professional practices adopted for patients who do not respond to medicinal and nonmedicinal treatments for behavioural disorders such as agitation, aggression, refusal and impulsive behaviour in a cognitive behavioural unit and show that valproic acid may provide an alternative. In fact, more patients benefited from VA and had a favourable clinical improvement entered in their medical record than those who benefited from VA but had an unfavourable medical observation in their record. These results of intermediate efficacy under VA were not confirmed in a significant manner by the NPI evaluation in our study. Additional studies are required to assess these effects quantitatively. As found in our study, VA causes excessive ammonia levels in the blood. This finding is described in the literature as triggering sedative effects, even drowsiness, with noteworthy neurological toxicity.[14] When treating behavioural disorders such as aggression, impulsive behaviour, agitation and refusal, such sedation could be confused with a beneficial treatment effect. We followed up these patients for the first time and showed that the clinical improvement in patients receiving valproic acid and discharged from the CBU with this treatment did not reveal higher blood ammonia levels than those recorded in patients discharged from the unit without VA. It therefore seems that if a patient experiences a clinical benefit with VA and ammonia levels in the blood are correct after treatment has been introduced, this alternative could be adopted as short- and long-term therapy. This study did not highlight an optimum patient profile to respond to valproic acid. However, the NPI score evaluating sleep imbalance was higher in the group of patients discharged without valproic acid. This can be interpreted as an unfavourable patient profile for initiating valproic acid treatment in a CBU. Finally VA seems to have a beneficial impact on concomitant prescriptions issued on discharge. In fact, psychotropic drugs can cause iatrogenic diseases in elderly subjects whilst antipsychotic agents can trigger substantial cardiovascular morbidity and mortality in this patient category (ref. geriatrics). According to this study, the inclusion of VA in the discharge prescription could reduce the number of neuroleptics and benzodiazepines prescribed.
To conclude, VA appears to be effective from a qualitative standpoint based on doctors’ evaluations whilst observing some patients presenting with behavioural disorders and admitted to a CBU. However, no quantitatively significant difference was confirmed with the NPI. The effect does not appear to be due to excessive ammonia levels in the blood and the sedation that this induces clinically. Finally, when tolerated and clinically effective, VA seems to reduce the administration of certain psychotropic agents and benzodiazepines which have proved deficient in the long-term treatment of the elderly.
REFERENCES
- Cesari M. Frailty: An Emerging Public Health Priority. J Am Med Dir Assoc 2016;17:188-92.
- Kazui H. Differences of Behavioral and Psychological Symptoms of Dementia in Disease Severity in Four Major Dementias. PloS ONE 2016;11:e0161092.
- Saidlitz P, Sourdet S, Vellas B, Voisin T. Management of behavioral symptoms in dementia in a specialized unit care. Geriatr Psychol Neuropsychiatr Vieil 2014;12:371-8.
- Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized. Placebo-controlled trials. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry 2006;14:191-210.
- Ballard C. Impact of antipsychotic review and non-pharmacological intervention on health-related quality of life in people with dementia living in care homes: WHELD-a factorial cluster randomised controlled trial. Int J Geriatr Psychiatry 2016.
- Haute Autorité de Santé Indicateurs de Pratique Clinique (IPC PMSA) 2016. Available at: http://www.has-sante.fr/portail/jcms/c_1250626/fr/indicateurs-de-pratique-clinique-ipc-pmsa
- Bialer M. Why are antiepileptic drugs used for nonepileptic conditions? Epilepsia 53 Suppl 2012;7:26-33.
- Taylor DM, Cornelius V, Smith L, Young AH. Comparative efficacy and acceptability of drug treatments for bipolar depression: a multiple-treatments meta-analysis. Acta Psychiatr. Scand 2014;130:452-69.
- Victoroff J, Coburn K, Reeve A, Sampson S, Shillcutt S. Pharmacological management of persistent hostility and aggression in persons with schizophrenia spectrum disorders: a systematic review. J Neuropsychiatry Clin Neurosci 2014;26:283-312.
- Epstein R. Psychosocial and Pharmacologic Interventions for Disruptive Behavior in Children and Adolescents. Agency for Healthcare Research and Quality US 2015.
- Xiao H, Su Y, Cao X, Sun S, Liang Z. A meta-analysis of mood stabilizers for Alzheimer’s disease. J Huazhong Univ Sci Technol Med Sci Hua Zhong Ke Ji Xue Xue Bao Yi Xue Ying Wen Ban Huazhong Keji Daxue Xuebao Yixue Yingdewen Ban 2010;30:652-8.
- Herrmann N, Lanctôt KL, Rothenburg LS, Eryavec G. A placebo-controlled trial of valproate for agitation and aggression in Alzheimer’s disease. Dement Geriatr Cogn Disord 2007;23:116-9.
- Porsteinsson AP. Divalproex sodium for the treatment of behavioural problems associated with dementia in the elderly. Drugs Aging 2006;23:877-86.
- Lewis C, Deshpande A, Tesar GE, Dale R. Valproate-induced hyperammonemic encephalopathy: a brief review. Curr Med Res Opin 2012;28:1039-42.