Self-medication: A current challenge
- *Corresponding Author:
- Dr. Darshana Bennadi
Department of Public Health Dentistry, Sree Siddhartha Dental College and Hospital, Agalkote, Tumkur - 572 107, Karnataka, India.
E-mail: darmadhu@yahoo.com
Abstract
Introduction: The ability of physicians to recognize non‑adherence is poor and interventions to improve adherence have had mixed results. Furthermore, successful interventions generally are substantially complex and costly. Poor adherence to medication regimens accounts for substantial worsening of disease; death and increased health care costs. The aim of this study is to assess the medication adherence in type‑2 diabetes patients who are on polypharmacy and the effect of counseling provided for them in a multispecialty hospital. Materials and Methods: The study was carried out at Kovai Medical Center and Hospital; Coimbatore Tamil Nadu, India. This is a 500‑bedded modernized, multi‑specialty tertiary care hospital with full‑fledged diabetic department. It caters to the needs of both out‑patients and in‑patients. An assessment was made on type‑2 diabetic patients who are receiving more than 5 drugs for their co‑morbidities were included in this study. A medication adherence questionnaire was prepared based on the literatures. The study was approved by the Kovai Medical Center and Hospital ethics committee. Results: Among 240 patients, 124 patients were adherent to medication whereas 116 patients were non‑adherent. The non‑adherent patients were giving verbal counseling in a private counseling room regarding medication adherence. Conclusions: Best way health professionals can tackle the adherence problem is through quality patient counseling as done in this study. With limited time most professionals have with a patient today this can be easier said than done. However, techniques such as the ask‑educate‑ask approach, the teach‑back method and motivational interviewing can help ensure patient understanding of the counseling provided.
icsatc neodeme advancedstructurescorp floormachinebrush scpe jcamasonry sages-tunisie sbsteel technomailleplus bolkan vaalea nsblueprinting mycleanairdoctors nycgeneralproroofing gabgadgets prsnekkern uniquescaffoldingsystems villaguicciardini acerpackaging acjstucco prontointervento-multiservice printersupplygiant sarel takkatiimi dragonshollow mazelsupply alfalchetto reliablegeneralagency lckenterprises realizzazione-giardini dmcindustries shop chathambrass ilfaroservizi soilmechanicsdrilling colorfullyyours agcsound carriere carnavaldetournai falconauto codingxcamp davinci-trondheim thebestofcolumbia cooperativetissage outsourcedmarketingpros tlc dawnnhough doubleclick pdirealty hattrennet az-bizsolutions jamaistropdart frontdata unitycreations fortisarezzo bspo-ken codar-confection theboulders bakerpersonnel fantasyphotographyandvideo fuleky tanssikoulutria ladybi swimanddance scuolavelatoscana x-pack creativeglazing lucagnizio sigaretteelettronichepisa mayiindustries frigo-clim elgars leoemma hotelalcantara el-pro therefore thebestofjacksonville nykran masmoudi thebestofspokane cogepre detrecruitment laresidencelepartage chimneycompanyboston awarepedia res-botanica recipefy semap thebestofcincinnati bb-one fourtech thebestofjoliet ajproduce jerryshulmanproduceshipper lckcabinetryny drivingtechniquesmadeeasy accademiaestetica pizzamaison schoonheidssalonbianca cabinsbrevardnc mrbrushes atlasrolloff hatip-medikal vezcocorporation thebestofcoloradosprings filtaclean monteleeper flyfisher ellatafa associazionepugliesiapisa unitycreationsltd maketeamstudiot douglasclear packagingpro softm allstarbeerinc burtonsupply footballscouting profondacreation johnvravickddsms fireislandbuilder advancedcontrolsolutions chittorgarhtaxiservices live-now orologeriatoscana racinemode thebestofwilmington agro-services violiner sandinghouse the-complete-package thebestofrichmond rcollision meubleskarray mes-recettes lawsandtaxes tavgrupp mkproducts royscottmarine taxi contreras-stockman sigmaweb de-noord thebestofkansascity maisonmedicaledelaeken recycledrubberpavers surfacingsystems unitedfidelityinc enokplan hunterremodeling edmersupply amerequipint sanilabcorp igglesis christiannursingregistry united-royal cantodelfiume northsidedeliny menuiserie-delbart passeritartufi justmyvoice ablefiresprinklers accantoalcentro ckperformance khalfallahpneus anti-flood-barriers bmstyle autosangiorgio-mercedes-benz carmagnino viipurinurheilijat multipack cma-eng mcafeerealty adrianaperciballi loconteedilecostruzioni konarprecision unityrubberco unityrubberproducts dante tela marathongranite baltimahalworcester heimdalbygg alstateprocessservice italydreamtour wemcocastingllc yachtbritesigns ecoledecroly-renaix anchorseniorapartments royalburton sk-veilag giannacapoti hubiteg customcommercialconstruction edm-nivelles probat-tunisie bachlawyer robertex inbora gpbconstruction tekstschrijver-tim bdsit trepro himalayanlounge lazersharpplumbing nycollisionking marinanova gealcorp nygabe maritimecoverage justmyvoice jukumech quimicolsa hayat-med aldrovandiauto michaelbenaltinc korenas sandvet americanmufflerautorepair justmyvoice liacoustics dminteriors agenziapromotech ligbtour internormfirenze justmyvoice zouila kohalmiferenc ashgroveresort ilmacinapepe suzukibandit hihna islandfishli prontointerventofabbro24h thebestofmidland thebestofportland dsgnaturaeambiente rimpex-medical giadaguidi royalroseappliances normas monicavignoliniluxury reddalsand defigners projektorilamput qtbservices labandas totalconceptdesign elannonnayttamo begmaterialiedili bardsdans samuelmanndds marksmenmfg demo17 chinafinewines coralia ivar-moe tournailesbains consew luisaprofumeriashop chimneycompanywestchester danapoly 268dental uspaerospace melonerp matcoservice emperorsoft cantare fninc greenpowerchemical westendsupply domobios unitysurfacingsystems martemoen hamptonssepticservices housatonicpaper sj-transport epsl-tunisie sungoldabrasives collinscreative barbarottomachinery soep thebestofalexandria straightlineconst itcimpianti hattrem-trafikkskole federalnetworks ppattorneys ceteau fbperformance coltgateway coolservice4u garaconfection bellformalwear abcconcretepumping mysantaria accurateindustrialmachining schmugerhardware thebestofjackson bellwetherstaffing sweetkarmadesserts tonerhuset mongilschool polycliniquelaouani buonidentro schoolbusmirrorsonline qlstransportation andereuropa cleanpressiondrycleaner bsyd planetlimony thebestoflasvegas csgmfoodequip potensial potiez invitiing tomscorvetteshop thebestbaltimorebusinesses honefoss thebestofoakland hydeparkdenim scmanndds sirreal totalpreferredsupply futureshockcorp myrtun
Keywords
Allopathic drugs, antibiotic resistance, self-medication
Introduction
Every day, we are practicing self-medication in the form of self-care of our health. [1] Around the 1960’s in the West-self-care and self-medication were regarded as unnecessary and potentially even unhealthy practices. This paternalistic approach to medicine, supported by health systems designed to treat sickness (rather than to prevent disease) remains a familiar aspect of health care in many countries to this day. [2]
Self-medication has traditionally been defined as “the taking of drugs, herbs or home remedies on one’s own initiative, or on the advice of another person, without consulting a doctor.” [3]
Families, friends, neighbors, the pharmacist, previous prescribed drug, or suggestions from an advertisement in newspapers or popular magazines are common sources of self-medications. Now-a-days, self-medication should be seen as the “desire and ability of people/patients to play an intelligent, independent and informed role, not merely in terms of decision-making but also in the management of those preventive, diagnostic and therapeutic activities which concern them.” [3-5]
Some governments are increasingly encouraging self-care of minor illnesses, including self-medication. Although responsible self-medication help to reduce the cost of treatment, travelling time as well as doctor’s time i.e., consultation time. [1,6]
Major problems related to self-medication are wastage of resources, increased resistance of pathogens and causes serious health hazards such as adverse reaction and prolonged suffering. Antimicrobial resistance is a current problem world-wide particularly in developing countries where antibiotics are available without any prescription. [1,7] Hence, the government should take necessary steps to regulate responsible self-medication. This can be done by making availability of safe drugs along with proper instructions about its use and if in need consulting a physician. [1,8]
In India, it is very common to see self-medication practice and which is emerging challenge to health care providers.
Extracting and synthesizing data
Articles which were published in peer reviewed journals, World Self-Medication Industry (WSMI) and World Health Organization (WHO) websites relating to self-medication reviewed.
Trend of “Rx-to-Over-the-Counter Switch”
The transfer of prescription (“Rx”) medicines to non-prescription or OTC status is known as the “Rx-to-OTC switch”. Many new medicines are first introduced as prescription medicines. After a sufficient time has passed in the use of the medicine by many patients and large-scale experience and scientific information has been gathered, for suitable conditions a manufacturer may elect to submit an application to the appropriate authority for the medicine to be given OTC status. [9]
Statistics
Studies carried out on self-medication states that it is very common practice, especially in economically deprived communities. Self-medication also has some advantages and dis advantages. [1,10]
Now-a-days health care services getting costlier and in developing countries health care facilities are not available. Hence, that time self-medication becomes an obvious choice of healthcare service. [1,11] Furthermore, it has been noted that purchase of drugs and many drugs that can only be purchased with prescription in developed countries are OTC in developing countries. In addition, lax medical regulation has resulted in the proliferation of counter free drugs that are in high demand for the treatment of highly prevalent diseases. [1,12]
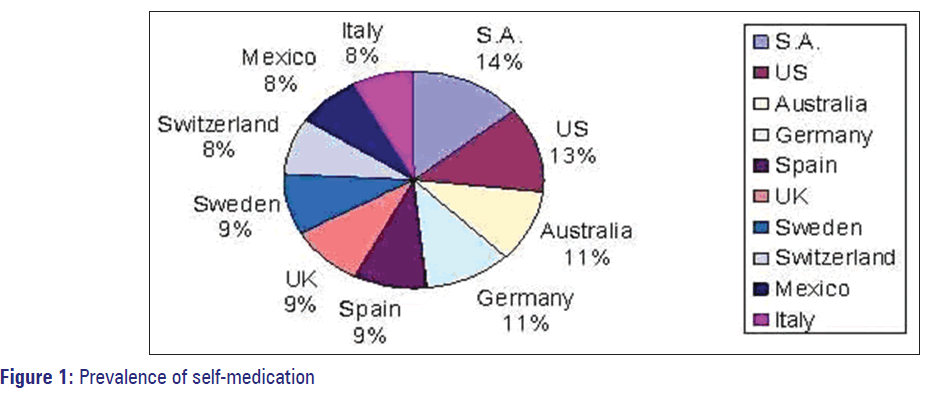
Self-medication is very common now a days and it is being used world-wide, given in [Figure 1]. [13]
India
Self-medication is very common among educated population. [14-19] In Punjab, the prevalence of self-medication was 73%.
Why do People Use Self-medication?
Modern consumers (patients) wish to take a greater role in the maintenance of their own health and are often competent to manage (uncomplicated) chronic and recurrent illnesses (not merely short-term symptoms) after proper medical diagnosis and with only occasional professional advice, e.g. use of histamine H2-receptor blocker, topical corticosteroid, antifungal and oral contraceptive. They are understandably unwilling to submit to the inconvenience of visiting a doctor for what they rightly feel they can manage for themselves, given adequate information. [20]
Self-medication is very common and a number of reasons could be enumerated for it. [18] Urge of self-care, feeling of sympathy toward family members in sickness, lack of time, lack of health services, financial constraint, ignorance, misbelieves, extensive advertisement and availability of drugs in other than drug shops are responsible for growing trend of self-medication. [19]
The Story of Self-care and Self-medication (1970-2010)
1970-The World Federation of Proprietary Medicine Manufacturers Association renamed as WSMI with an objective to stress for world-wide regulatory classification of medicinal products into two classes: Prescription and non-prescription. [21]
1975-First international symposium on the role of the individual in primary care was held at the European Regional Offices of the WHO-stress on “self-care”. [21]
1977-World Health Assembly adopted the resolution calling for “health for all” by the year 2000 and in 1978, the Declaration of Alma-Ata. [21]
1981-World Medical Association stressed the responsibility of people for their own health in a “Declaration on the Rights of the Patient.” [21]
1986-Ottawa (Canada) and launched “the Ottawa Charter for Health Promotion”, in which self-care was identified as one of the three key mechanisms for health promotion. [21]
A new era of access to modern, effective medicines was heralded in the early 1980s, when medicines which had previously only been available on prescription began to be switched to non-prescription status. Among the first products switched to non-prescription status was ibuprofen for the treatment of pain, in the UK (1983) and the US (1984). In Canada, hydrocortisone became available without a prescription in 1986. A statement of WSMI Policy on Consumer Information and the Role of Labeling was formally approved and released by the WSMI Board of Directors at the Fifth General Assembly in October 1979 in Australia. The policy emphasizes that the role of labeling is “to provide all information necessary to enable an individual without medical training to use the medicine appropriately.” [21]
The 1990’s-Guiding Principles in Self-Medication
1990’s, there was an increasing recognition in many parts of the world that people were managing or treating a large proportion of their ailments without always consulting a health professional. [21]
1998, Role of pharmacist in self-medication was explained by WSMI and the International Pharmaceutical Federation (FIP). [21]
1993-WSMI’s 11th General Assembly in Acapulco, Mexico, where the theme is “Globalization of the self-medication market: challenges and opportunities.” [21]
1997-WSMI publishes its first global review of consumer surveys: “Health care, self-care and self-medication.” [21]
1999-A joint statement is produced by WSMI and FIP entitled “responsible self-medication”.
WSMI’s 13th General Assembly in Berlin, Germany, where the theme is “self-care, a vital element of health policy in the information age.” [21]
2000-2005-The Benefits of Responsible Self-Medication
2000-2005-The Benefits of Responsible Self-Medication
2006-2010 and the future-A globalizing world. Prevention of disease through self-care and responsible self-medication. [21]
Sources
The common sources of self-medication are previous prescription, friends, advertisements, chemist shop and books. [14-17]
Factors influencing
Self-medication is influenced by many factors such as education, family, society, law, availability of drugs and exposure to advertisements. [1,22,23] Table 1 shows list of drugs used for self-medication. [24,25]
| Category | Drugs |
|---|---|
| Cough and cold | D-cold total, corex, benadryl, glycodin |
| Analgesics | Saridon, disprin, diclofenac, nimesulide, |
| paracetamol, ibuprofen | |
| Antipyretics | Calpol, crocin |
| Antiseptic | Dettol, boroplus |
| Antibiotics | Ciprofloxacin, norfloxacin, amoxicillin, cefadroxil |
| Others | Dabur chyawanprash |
Table 1: List of drugs used for self-medication
Potential benefits
Individual level
• An active role in his or her own health care
• Self-reliance in preventing or relieving minor symptoms or conditions
• Education opportunities on specific health issues (i.e. stop smoking aids and products to treat heartburn)
• Convenience
• Economy, particularly since medical consultations will be reduced or avoided. [26]
At community level
Good self-medication can also provide benefits such as:
• Saving scarce medical resources from being wasted on minor conditions
• Lowering the costs of community funded health care programs
• Reducing absenteeism from work due to minor symptoms
• Reduce the pressure on medical services where health care personnel are insufficient
• Increase the availability of health care to populations living in rural or remote areas. [26]
In a world of scarce government and in many countries scarce individual resources, responsible self-medication should be a cornerstone of healthcare provision and health policy. [26]
Potential risks
Individual level
• Incorrect self-diagnosis
• Failure to seek appropriate medical advice promptly
• Incorrect choice of therapy
• Failure to recognize special pharmacological risks
• Rare but severe adverse effects.
• Failure to recognize or self-diagnosis contraindications, interactions, warnings and precautions
• Failure to recognize that the same active substance is already being taken under a different name
• Failure to report current self-medication to the prescribing physician (double medication/harmful interaction)
• Failure to recognize or report adverse drug reactions
• Incorrect route of administration
• Inadequate or excessive dosage
• Excessively prolonged use
• Risk of dependence and abuse
• Food and drug interaction
• Storage in incorrect conditions or beyond the recommended shelf life. [26]
Community level
Improper self-medication could result in an increase in drug induced disease and in wasteful public expenditure. [26]
Prevention of Potential Risks Associated with Self-medication
Role of health profession
Health professionals are one who has potential role in preventing risks of self-medication. Because he is the one who work on three main therapeutic aspects of professionalism in his daily practice: Information, therapeutic advice and education. [3]
Information
Whenever health professionals are prescribing drugs, he should give proper instructions and explain for what it is prescribed so that it will be helpful for the patient to understand and making his own decisions. Given information should be at patient’s comprehension level so that it will be helpful for them to understand its management. [3]
Therapeutic advice
Lack of therapeutic compliance is a serious problem in both acute and chronic treatments and reflects a poorly-understood or incomplete description of the treatment aims. If patients are not well-informed they are unlikely to use medication correctly. However, if the directions for use and the limitations of a given drug are explained-for example, dose, frequency of dose, treatment course, how to take it, etc., then patients have a set of guidelines which will help them to use the drug correctly, both now and in the future. Inappropriate and erratic self-medication, along with lack of compliance, will only be reduced if patients are informed and understand clearly why certain advice has been given. [3]
Education
Inappropriate self-medication is the result of the medical model from which people have learnt. Proper health education should be given to the patients. By regularly adopting an educational attitude we can have an effect on large sectors of the population, on people who, in turn, may directly influence their friends and family. This aspect is of particular importance with respect to the self-medication of children by their parents or takes cares. [3]
Role of pharmacist
He is one of the key role players in educating his customers about the proper use of medicines, which are intended for self-medication. For that necessary steps have to be taken in his training and practice. [27]
Pharmacists play a valuable role in identifying, solving and preventing drug-related problems for the purpose of achieving optimal patient outcomes and quality of life. Ambulatory based pharmacists have the opportunity and responsibility to foster safe, appropriate, effective and economical use of all medications, especially those therapies patients are self-selecting. Pharmacists should guide their customers to consult the physician before taking any medication by self. [28,29,30] Unlike above role, pharmacists have following function as a:
Communicator
In order to address the condition of the patient appropriately the pharmacist must ask the patient key questions and pass on relevant information to him or her (e.g. How to take the medicines and how to deal with safety issues). [3,31]
Quality drug supplier
The pharmacist must ensure that the products he/she purchases are from reputable sources and of good quality. [3,31]
Trainer and supervisor
To achieve this pharmacist must develop a protocol for referral to the pharmacist, protocols for community health workers involved with the handling and distribution of medicines. [3,25,31]
Collaborator
It is imperative that pharmacists develop quality collaborative relationships with the other health care professionals, national professional associations, the pharmaceutical industry, governments (local/national), patients and general public. [3,31,32]
Health promoter
As a member of the health-care team, the pharmacist must participate in health screening to identify health problems and those at risk in the community, participate in health promotion campaigns to raise awareness of health issues and disease prevention, provide advice to individuals to help them make informed health choices. [3,31]
Promotion of Responsible Self-Medication
The OTC Committee of the Organization of Pharmaceutical Producers of India is working toward the promotion of responsible self-medication with a view to grow the OTC sector. It is aiming to get regulatory support for issues such as the accessibility of household TC remedies and increasing the awareness of the importance of responsible self-medication with the general public and the government. [33]
Many healthcare organizations have made important statements on self-care and self-medication, singly or jointly with WSMI. Some selected illustrations only are given here: [9]
The WHO: “It has become widely accepted that self-medication has an important place in the health care system. Recognition of the responsibility of individuals for their own health and awareness that professional care for minor ailments is often unnecessary has contributed to this view. Improvements in people’s general knowledge, level of education and socio-economic status in many countries form a reasonable basis for successful self-medication.” (Guidelines for the regulatory assessment of medicinal products for use in self-medication. 2000). [9]
The FIP: “To have good health, people are becoming more responsible, getting proper information as much as possible to decide in their own care. Pharmacists and the manufacturers of non-prescription medicines share the common goals of providing high quality service to the public and encouraging the responsible use of medicines.” (Joint Statement by The FIP and the WSMI, 1999). [9]
The international council of nurses (ICN): “Self-medication is a key component of self-care that is particularly significant in an era of increasing chronic illness and well-informed health care consumers. Optimizing responsible self-medication is an important and underused resource for health and provides an opportunity for collaboration and consultation among consumers, nurses, pharmacists and physicians.” (Joint Statement by the ICN and the WSMI, 2003). [9]
Conclusion
Self-medication is an alarming concept. This review focused on the self-medication of allopathic drugs, their use, its safety and reason for using it. It would be safe, if the people who are using it, have sufficient knowledge about its dose, time of intake, side-effect on over dose, but due to lack of information it can cause serious effects such as antibiotic resistance, skin problem, hypersensitivity and allergy. Hence, developing country like India where we have poor economic status, education status as well as poor health care facilities. People have less knowledge regarding risks associated with their self-medication. We are on the edge of sword whether to promote self-medication or not. Hence it is recommended that holistic approach should be taken to prevent this problem, which includes proper awareness and education regarding the self-medication and strictness regarding pharmaceutical advertising. Dispensing modes in the needs to be improved through proper education, strict regulatory and managerial strategies to make health care easily accessible and cost-effective. [1]
Health professionals have to spend some extra time in educating patients regarding the same. Improved knowledge and understanding about self-medication may result in rationale use and thus limit emerging microbial resistance issues.
References
- Vizhi SK, Senapathi R. Evaluation of the perception, attitude and practice of self-medication among business students in 3 select Cities, South India. International Journal of Enterprise and Innovation Management Studies (IJEIMS) July-December 2010;1 (3): 40-4.
- Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self-medication. Drug Saf 2001;24: 1027-37.
- Hernandez-Juyol M, Job-Quesada JR. Dentistry and self-medication: A current challenge. Med Oral 2002;7:344-7.
- Laporte JR, Castel JM. The physician and self-medication. Med Clin (Barc) 1992;99:414-6.
- Laporte JR. Self-medication: Does information to users increase at the same rate as consumption. Med Clin (Barc) 1997;109:795-6.
- Porteous T, Bond C, Hannaford P, Sinclair H. How and why are non-prescription analgesics used in Scotland? Fam Pract 2005;22:78-85.
- Pagán JA, Ross S, Yau J, Polsky D. Self-medication and health insurance coverage in Mexico. Health Policy 2006;75:170-7.
- World Health Organization: Report of the WHO Expert Committee on National Drug Policies 1995. Available from: http://www.who. int/medicines/library/dap/who-dap-95-9/who-dap-95.9.shtml. [Last accessed on 8-9-2010] Available from: http://www.wsmi.org/news/news_113.htm. [Last accessed on 2012 Jan 10].
- Geissler PW, Nokes K, Prince RJ, Odhiambo RA, Aagaard-Hansen J, Ouma JH. Children and medicines: Self-treatment of common illnesses among Luo schoolchildren in western Kenya. Soc Sci Med 2000;50:1771-83.
- Chang FR, Trivedi PK. Economics of self-medication: Theory and evidence. Health Econ 2003;12:721-39.
- Shakoor O, Taylor RB, Behrens RH. Assessment of the incidence of substandard drugs in developing countries. Trop Med Int Health 1997;2:839-45.
- Available from: http://www.abimip.org.br/uploads/material_de_ apoio/1296056417_792.pdf/. [Last accessed on 2011 Dec 28].
- Verma RK, Mohan L, Pandey M. Evaluation of self-medication among professional students in North India: Proper statutory drug control must be implemented. Asian J Pharm Clin Res 2010;3:60-4.
- Shveta S, Jagmohan S. A study of self-medication pattern in Punjab. Indian J Pharm Pract 2011;4:43-8.
- Joshi MC, Shalini, Agarwal S. A questionnaire based study of self-medication practices among young population. Res. J. Pharm., Biol. Chem. Sci. 2011;2:761-6.
- Sharma R, Verma U, Sharma CL, Kapoor B. Self-medication among urban population of Jammu city. Indian J Pharmacol 2005;37:37-45.
- Solomon W, Abede GM. Practice of self-medication in Jimma Town. Ethiop J Health Dev 2003;17:111-6.
- Phalke VD, Phalke DB, Durgawale PM. Self-medication practices in rural Maharashtra. Indian J Community Med 2006;31:34-5.
- Student lancet. Available from: http://www.thelancetstudent. com. [Last accessed on 2010 Sep 8].
- Available from: http://www.wsmi.org/pdf/storyofselfcare_bdpage.pdf. [Last accessed on 2012 Jan 15].
- Montastruc JL, Bagheri H, Geraud T, Lapeyre-Mestre M. Pharmacovigilance of self-medication. Therapie 1997;52:105-10.
- Habeeb GE Jr, Gearhart JG. Common patient symptoms: Patterns of self-treatment and prevention. J Miss State Med Assoc 1993;34:179-81.
- Jain S, Malvi R, Purviya JK. Concept of self-medication: A review. Int J Pharm Biol Arch 2011;2:831-6.
- Ruiz ME. Risks of self-medication practices. Curr Drug Saf 2010;5:315-23.
- Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva: WHO; 2000.
- Available from: http://www.apps.who.int. [Last accessed on 2010 Sep 8]. 28. Wilbur K, Salam SE, Mohammadi E. Patient perceptions of pharmacist roles in guiding self-medication of over-the-counter therapy in Qatar. Patient Prefer Adherence 2010;4:87-93.
- General Information WHO Drug Information. Vol. 14, No. 1, 2000. Available from: http://www.apps.who.int. [Last accessed on 2010 Sep 8].
- Available from: http://www.whqlibdoc.who.int/hq/1998/WHO_ DAP_98.13.pdf. [Last accessed on 2011 Dec 28].
- Role of the pharmacist in the health care system. Available from: http:// www.apps.who.int. [Last accessed on 2010 Sep 9].
- Available from: http://www.pharmahost.org. [Last accessed on 2010 Sep 8].
- Available from http://www.indiaoppi.com/IndiaOTCpharmaProfile2011. pdf. [Last accessed on 2011 Dec 28].