Risk of Obstructive Sleep Apnea (OSA) Assessment among Patients with Type 2 Diabetes in Taif, Saudi Arabia
2 College of Pharmacy, Taif University, Taif, Saudi Arabia
Citation: Kalakattawi RM, Kalakattawi AM, Alsuqati FA et al. Risk of Obstructive Sleep Apnea (OSA) Assessment among Patients with Type 2 Diabetes in Taif, Saudi Arabia. J Basic Clin Pharma 2018;9:65-67.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
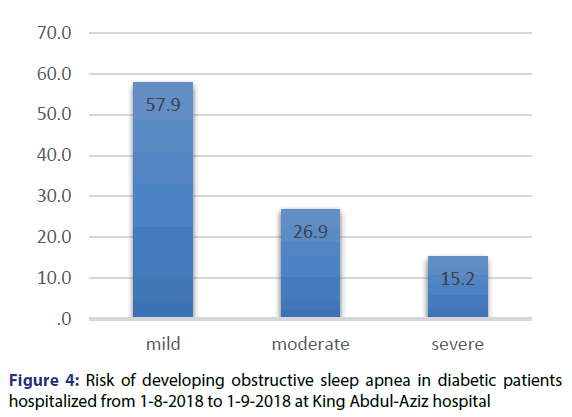
Background: Obstructive sleep apnea (OSA) is a common condition in middleaged persons worldwide. The major factor risk of this disease is obesity. Methods: A cross sectional study was performed at king Abdul-Aziz hospital. A STOP-BANG questionnaire formed of eight questions was used to assess the risk of OSA among type 2 diabetic patients. The scoring scale is categorized into three groups: low, intermediate and high 0-2, 3-4 and 5-8 respectively. By this study, we aimed to assess the risk of OSA among diabetes patients in Taif city. Results: 57.9% of patients had mild risk, 26.9% had moderate risk and 15.2% had severe risk for OSA. There was a moderate positive relationship between age and STOP-BANG score. There was no significant correlation between the score and Last fasting blood sugar and HbA1C’s level, with p-value=0.554 and 0.335 respectively. There was a significant relationship between the type of treatment and the risk of developing OSA (p-value<0.001). Percentage of patients with severe risk was significantly higher in those taking both insulin and oral drugs than those taking insulin alone or oral drugs alone. Conclusions: The OPA risk and prevalence is much higher in diabetics than in general population, with the risk increasing with age. The risk is higher in diabetic patients who are receiving both oral hypoglycemic drugs and insulin. The screening of OSA among diabetic patients is necessary to identify those at severe risk and manage this problem, which may remain undiagnosed in many patients.
Keywords
Obstructive sleep apnea; type 2 DM; diabetes; Saudi Arabia
Introduction
Obstructive Sleep Apnea (OSA) is a repetitive episode of partial and complete airway obstructions during sleep. This disorder can be caused by common type of sleep disorders and this condition is associated with oxyhemoglobin desaturations.[1,2] The prevalence of OSA increases with aging. In men and women between 30 and 60 years old, the prevalence is 24% in men and 9% in women. OSA is common in both developing and developed countries and its prevalence has increased in the last two decades.[3] Most studies reported a 1.5- to 3-fold higher prevalence of OSA in men.[4] The OSA has a number of risk factors, the most important is obesity reflected by BMI, neck circumference and waist to hip ratio.[5,6] Other risk factors have been reported in the literature as aging, male gender, genetic predisposition, smoking, alcohol drinking and craniofacial anomalies.[7,8]
Cross-sectional studies indicate an association between OSA and certain medical conditions like diabetes mellitus type 2, hypertension, heart failure, coronary heart disease and polycystic ovary syndrome. [9-11] OSA could be novel risk factor of type 2 diabetes or vice versa.[12] The glucose control in diabetics with OSA is poor and the severity of OSA is directly related to hemoglobin A1C values.[13] Studies reported a significant association between Insulin resistance and sleep apnea in general population independently of any confounder especially obesity.[14-16]
In a study conducted to test the effect of OSA treatment in diabetic patients the authors found that insulin sensitivity enhanced after using of continuous positive airway pressure after two nights of treatment, this was obvious in patient with BMI less than 30 kg/m2.[17]
Methodology
Objective
We aimed to assess the risk of OSA among diabetic patients hospitalized from June to August 2018 at King Abdul-Aziz specialist hospital in Taif city - Saudi Arabia.
Study design
Cross sectional observational study.
Study sample
Inclusion criteria
Patients hospitalized from 1-6-2018 to 1-8-2018 at King Abdul-Aziz specialist hospital in Taif city and diagnosed with type 2 diabetes mellitus.
Exclusion criteria
The patients with type 1 diabetes or patients who did not have type 2 were excluded.
Data collection
Data were collected using the STOP BANG Sleep Apnea screening questionnaire.[18] The questionnaire includes 8 dichotomous questions that offer an easy method to assess the risk of OSA [Table 1]. The scoring scale is categorized into three groups; low, intermediate and high 0-2, 3-4 and 5-8 respectively. The yes answer=1 and no=0. Total score=8.
| Stop | Yes | No |
|---|---|---|
| Do you SNORE loudly (louder than talking or loud enough to be heard through closed doors)? | Yes | No |
| Do you often feel TIRED, fatigued, or sleepy during daytime? | Yes | No |
| Has anyone OBSERVED you stop breathing during your sleep? | Yes | No |
| Do you have or are you being treated for high blood PRESSURE? | Yes | No |
| Bang | Yes | No |
| BMI more than 35 kg/m2? | Yes | No |
| AGE over 50 years old? | Yes | No |
| NECK circumference >16 inches (40 cm)? | Yes | No |
| GENDER: Male? | Yes | No |
Table 1: The STOP-Bang Questionnaire
Other collected variables
Other co-morbidities such as hypertension, coronary heart disease, heart failures, stroke or others. Oral medication or insulin injection. HgA1C. Last fasting blood sugar.
Statistical analysis
To describe qualitative variables frequency and percentage were used. The mean, the median and the standard deviation were used to describe quantitative variables. To test the relationship between the score and quantitative variables spearman correlation was used. To analyse the association between the level of OSA’s risk and the type of treatment of diabetes chi square test was used. The significant level of p was fixed at 0.05.
Results
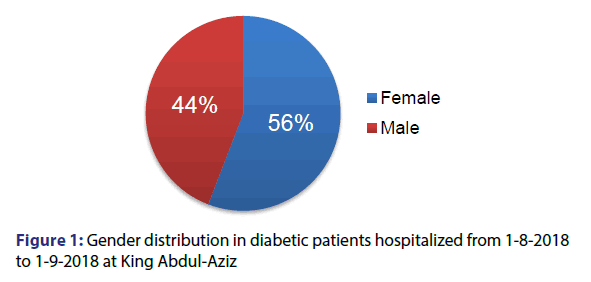
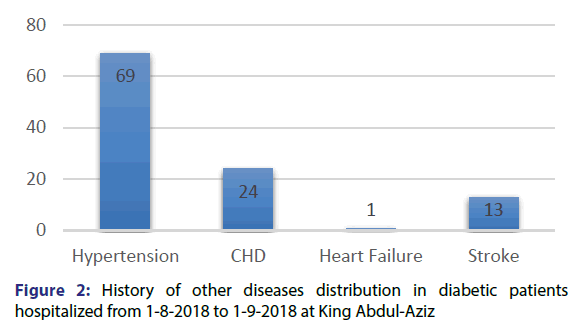
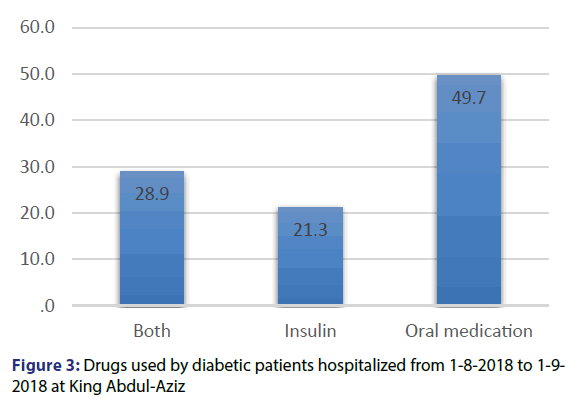
197 patients participated in our study, 55.8% of them were females and 44.2% were males [Figure 1]. The mean age of the participants was 56.1 years and the standard deviation was 15.5 years. The minimum age was 12 years and the maximum was 93 years. Among our patients, 35% had hypertension, 12.2% had history of coronary heart disease and 6.6% had history of stroke. Only one patient had heart failure [Figure 2]. As regards to diabetes treatment, 49.7% of the patients were using oral hypoglycaemic drugs, while 21.3% were using Insulin, 28.9% of the patients are using both insulin and oral hypoglycaemic drugs [Figure 3]. Most of the patients participating in the study (166) were able of remembering their last FBS reading, where the mean reading was 189.7 mmol/l and the standard deviation was 75.8 mmol/l. For the HBA1C, 166 patients mentioned their reading with the mean 8.6% and the standard deviation was 2%.
The score of STOP-BANG questionnaire was calculated for all the patients and the mean was 2.6 and the standard deviation was 1.7 and the median was 2 [Table 2]. Patients’ risk was calculated based on the score of STOP-BANG questionnaire, and the result was that 57.9% of the patients had mild risk, 26.9% had moderate risk and 15.2% had severe risk of OSA [Figure 4].
| N | Minimum | Maximum | Median | Mean | Std. Deviation | |
|---|---|---|---|---|---|---|
| Total score | 197 | 0 | 7 | 2 | 2.56 | 1.724 |
Table 2: STOP-BANG questionnaire score in diabetic patients hospitalized from 1-8-2017 to 1-9-2017 at King Abdul-Aziz
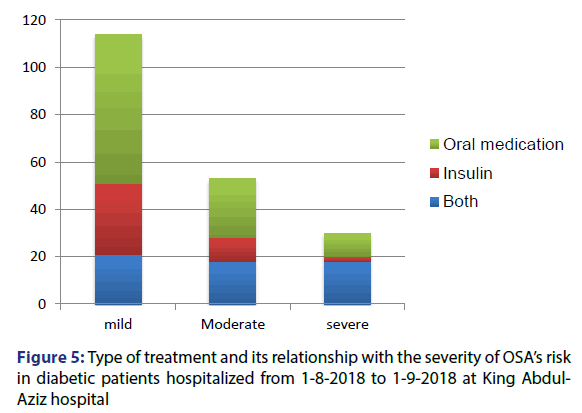
Spearman’s correlation was calculated for the relationship between the score and the age which was significant with p-value < 0.001, the correlation coefficient was 0.35. Spearman’s correlation was also calculated for the FBS and the HbA1C, but it was non-significant with p-value=0.554 and 0.335 respectively. Chi square test was performed to test for the presence of relationship between the type of treatment and the risk severity of developing OSA, it was significant with p-value < 0.001. Percentage of patients with severe risk was higher in those taking both insulin and oral drugs than in those taking insulin alone or oral drugs alone [Figure 5].
Discussion
A total of 197 diabetic patients participated in our study aiming at assessing the risk of obstructive sleep apnea in the diabetic patients in Taif city. The measurement tool used in this study was the STOPBANG questionnaire. The score of STOP-BANG questionnaire was calculated for all the patients and the mean was 2.6 and the standard deviation is 1.7. According to the scores of the patients, 57.9% of patients had mild risk, 26.9% had moderate risk and 15.2% had severe risk for OSA. A significant correlation was found between the score and the age and the correlation coefficient was 0.35 meaning that there is a moderate positive relationship between age and the score. There was no significant correlation between the score and FBS’s level and between the score and the HbA1c’s value.
The presence of relationship between the type of the treatment of the diabetes and the risk severity of developing OSA was tested and it was significant with p-value < 0.001. Percentage of patients with severe risk was higher in those taking both insulin and oral drugs than those taking insulin alone or oral drugs alone. The results of this study can be compared to those of a study published in 2006 and studying the prevalence of obstructive sleep apnea (OSA) in men with type 2 diabetes.[19] The authors found that 57% were scored as “high†and 39% as “low†risk for OSA; 4% were already known to have OSA. The method used in this study is a questionnaire different from the STOPBANG questionnaire. There was no significant difference in HbA1c levels between the “high†and “low†risk groups, which is the same result we reached in our study.
One other study focused on Obstructive Sleep Apnea among Obese Patients with Type 2 Diabetes. It showed that over 86% of participants had OSA with an apnea-hypopnea index (AHI) = 5 events/h. The mean AHI was 20.5 ± 16.8 events/h. A total of 30.5% of the participants had moderate OSA (15 = AHI<30), and 22.6% had severe OSA (AHI = 30).[20] In a study conducted to test the relationship between sleep-disordered breathing and insulin resistance, authors found that sleep-disordered breathing parameters (AHI and minimum oxygen saturation) were independent determinants of insulin resistance.[21] A based population study performed in 1,387 participants of the Wisconsin Sleep Cohort found a significant association between sleep apnea and type 2 diabetes this relationship was independent from other risk factors.[22]
Conclusion
In conclusion, the OPA risk and prevalence is much higher in diabetics than in general population, with the risk increasing with age. The risk is higher in diabetic patients who are receiving both oral hypoglycaemic drugs and insulin. These results suggest that the screening of OSA among diabetic patients is necessary to identify those at severe risk and managing this problem, which may remain undiagnosed in many patients.
REFERENCES
- Lam JC, Sharma SK, Lam B. Obstructive sleep apnoea: definitions, epidemiology and natural history. Ind J Med Res 2010;131:165-70.
- Patil SP, Schneider H, Schwartz AR, Smith PL. Adult obstructive sleep apnea: pathophysiology and diagnosis. Chest 2007;132:325-37.
- Garvey JF, Pengo MF, Drakatos P, Kent BD. Epidemiological aspects of obstructive sleep apnea. J Thorac Dis 2015;7:920-9.
- Naresh M. The Epidemiology of Adult Obstructive Sleep Apnea. Proc Am Thorac Soc 2008;5:136-43.
- Tishler PV, Larkin EK, Schluchter MD. Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. JAMA 2003;289:2230-7.
- Al-Lawati NM, Patel SR, Ayas NT. Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Prog Cardiovasc Dis 2009;51:285-93.
- Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep apnea in adults. JAMA 2004;291:2013-6.
- Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population a review on the epidemiology of sleep apnea. J Thorac Dis 2015;7:1311-22.
- Foster G, Kuna ST, Sanders M. Sleep apnea in obese adults with type 2 diabetes: baseline results from the Sleep AHEAD study. Sleep 2005;28:A606.
- Fogel RB, Malhotra A, Pillar G, Pittman SD, Dunaif A, White DP, et al. Increased prevalence of obstructive sleep apnea syndrome in obese women with polycystic ovary syndrome. J Clin Endocrinol Metabol 2001;86:1175-80.
- Logan AG, Perlikowski SM, Mente A, Tisler A, Tkacova R, Niroumand M, et al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens 2001;19:2271-7.
- Pamidi S, Tasali E. Obstructive Sleep Apnea and Type 2 Diabetes: Is There a Link? Front Neurol 2012;3:126.
- Aronsohn RS, Whitmore H, Van Cauter E, Tasali E. Impact of Untreated Obstructive Sleep Apnea on Glucose Control in Type 2 Diabetes. Am J Respir Crit Care Med 2010;181:507-13.
- Punjabi NM, Shahar E, Redline S. Sleep-disordered breathing, glucose intolerance, and insulin resistance: The Sleep Heart Health Study. Am J Epidemiol 2004;160:521-30.
- Theorell HJ, Berne C, Janson C. Obstructive sleep apnoea is associated with decreased insulin sensitivity in females. Eur Respir J 2008;31:1054-60.
- Punjabi NM, Beamer BA. Alterations in Glucose Disposal in Sleep-disordered Breathing. Am J Respir Crit Care Med 2009;179:235-40.
- Harsch IA, Schahin SP, Radespiel Tröger M, Weintz O, Jahreiß H, Fuchs FS, et al. Continuous Positive Airway Pressure Treatment Rapidly Improves Insulin Sensitivity in Patients with Obstructive Sleep Apnea Syndrome. Am J Respir Crit Care Med 2004;169:156-62.
- Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest 2016;149:631-8.
- West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax 2006;61:945-50.
- Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, et al. Obstructive Sleep Apnea Among Obese Patients With Type 2 Diabetes. Diabetes Care 2009;32:1017-9.
- Ip MS, Lam B, Ng MM. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med 2002;165:670-6.
- Reichmuth KJ, Austin D, Skatrud JB. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med 2005;172:1590-5.