Protective effect of hesperidin on cardiovascular complication in experimentally induced myocardial infarction in diabetes in rats
- *Corresponding Author:
Date of Received: 16-02-2010
Date of Modified: 22-03-2010
Date of Accepted: 19-04-2010
Available Online: 15-05-2010
Abstract
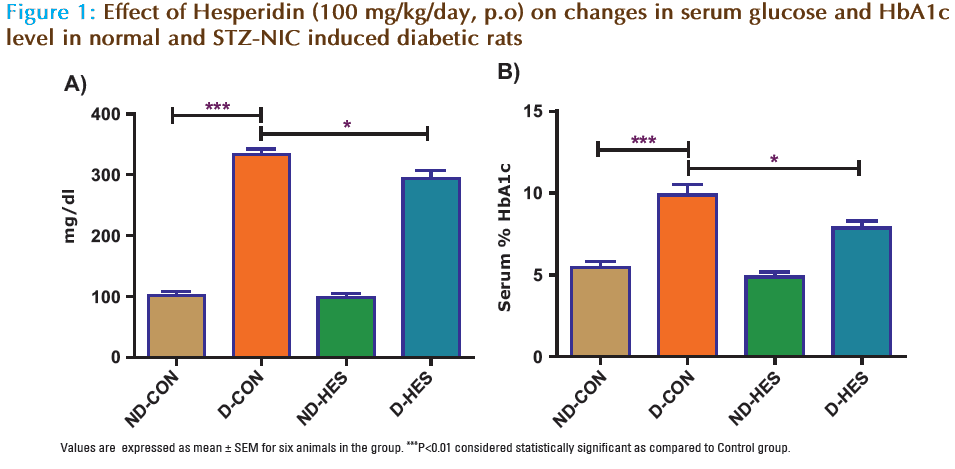
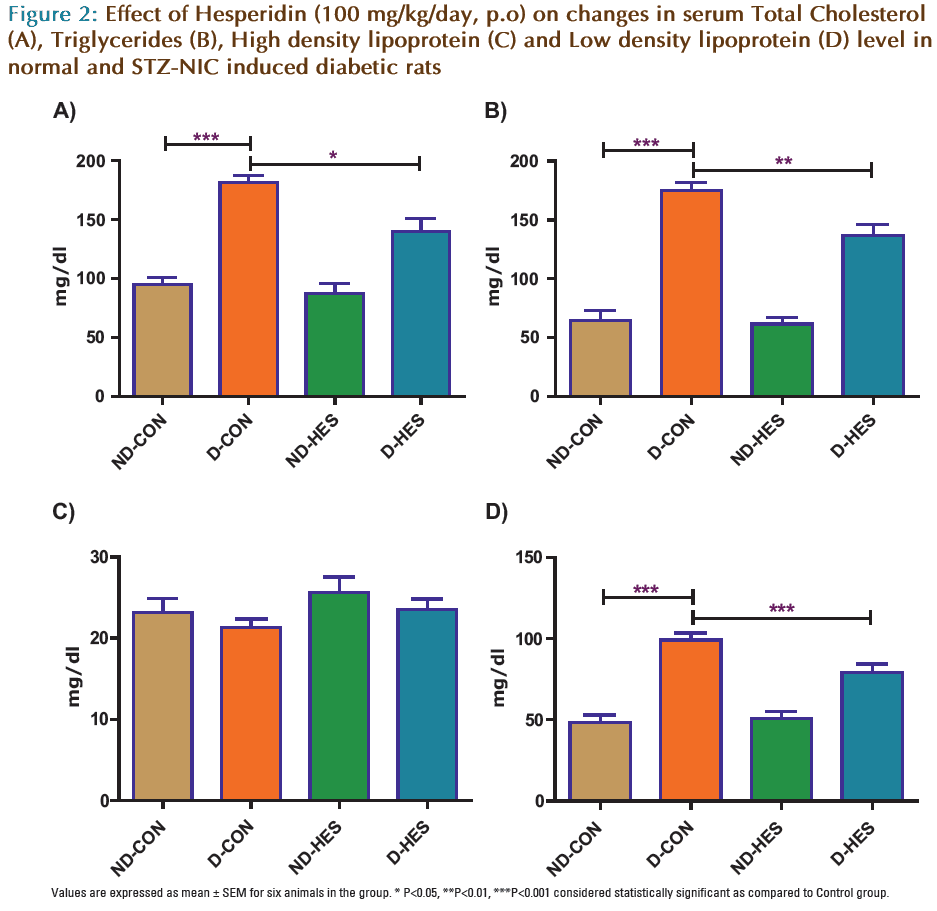
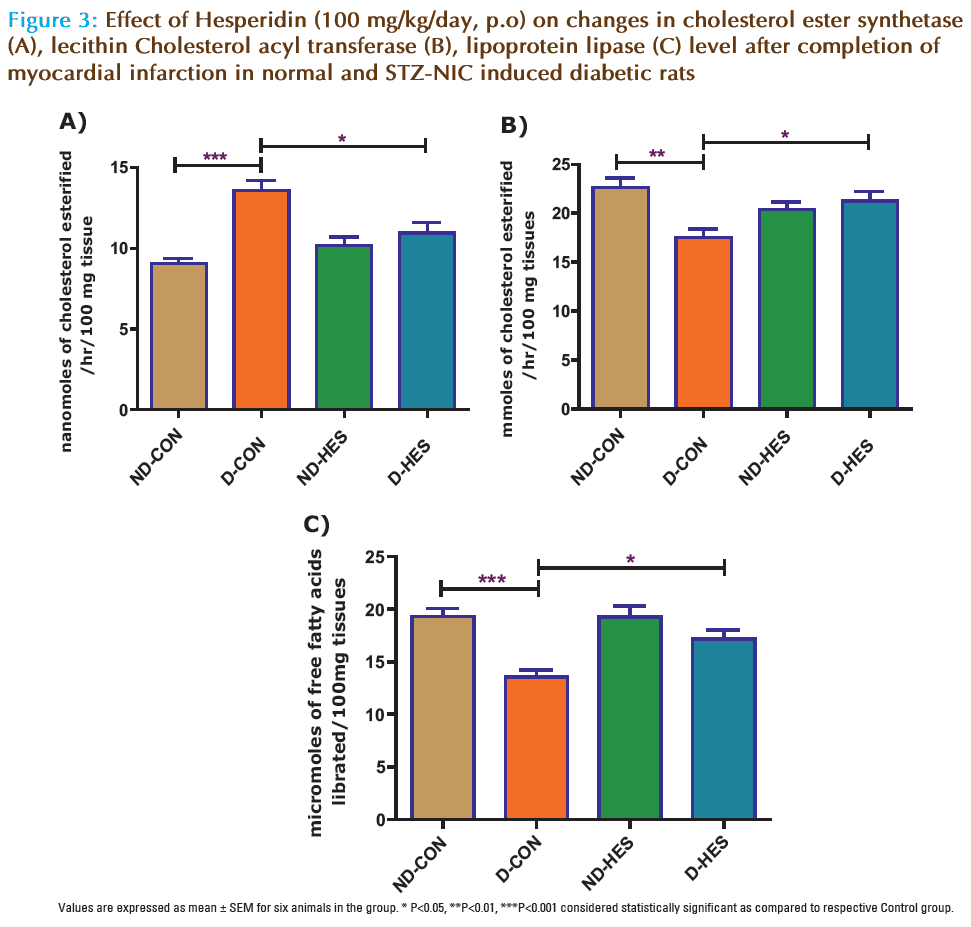
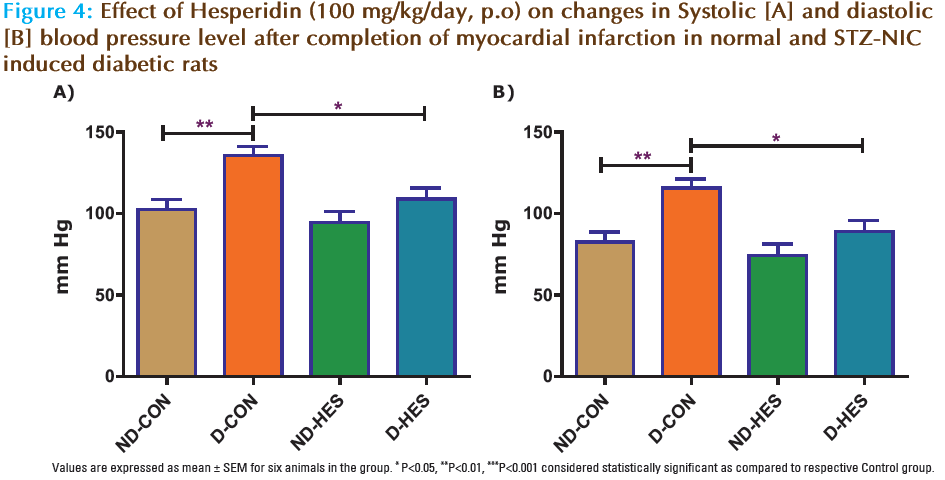
Present study was designed to evaluate effect Hesperidin on Cardiovascular Complication in isoproterenol induced myocardial infarction in normal and Streptozotocin-Nicotinamide induced in diabetic rats. Hesperidin (100 mg/kg, p.o) was administered for 28 days in rats injected with single dose of Streptozotocin (65 mg/kg, i.p, STZ) and Nicotinamide (110 mg/kg, i.p, NIC) and after isoproterenol (200 mg/kg, s.c.) induced myocardial infarction in rats on 29th and 30th day. At the end of experimental period (i.e. on the day 31) serum and heart tissues sample were collected, and glucose, HbA1c and Total Cholesterol (TC), Triglycerides (TG) and High density lipoprotein (HDL) and cholesterol ester synthetase (CES), lecithin Cholesterol acyl transferase (LCAT), lipoprotein lipase (LPL), systolic and diastolic blood pressure were find out. Administration of STZ–NIC in rats showed a significant (p<0.001) increased in the levels of serum glucose, glycosylated heamoglobin (HbA1c), Total Cholesterol (TC), Triglycerides (TG) and Low density lipoprotein (LDL) whereas the levels of High density lipoprotein (HDL) were found to be non significant but significant (p<0.001) increased in the level of heart tissues CES and significant (p<0.001, p<0.01) decreased LCAT and LPL, significantly (p<0.01) increased systolic and diastolic blood pressure as compared to respective control groups. Treatment with Hesperidin significantly (P<0.05) decreased HbA1c, glucose, CES level and significantly (P<0.01) decreased LDL, TC, TG, systolic and diastolic blood pressure and significant (P<0.01) increased LCAT and LPL level but no significantly change HDL in compared to diabetic control group. We concluded that HES (100 mg/kg) is effective in controlling blood glucose levels and reduced cardiac complication in experimentally induced myocardial infarction diabetic rats.
Keywords
Hesperidin, Streptozotocin, Nicotinamide, lipid profile, blood pressure
Introduction
Three major metabolic abnormalities contribute to the development of hyperglycemia in Type 2 diabetes mellitus such as impaired insulin secretion in response to glucose, increased hepatic glucose production and decreased insulinstimulated glucose uptake in peripheral tissues. The latter 2 abnormalities are primarily due to insulin resistance [1,2]. Non insulin dependent diabetic mellitus has also been associated with an increased risk for premature arteriosclerosis due to increase in triglycerides and low density lipoprotein levels. About 70-80% of deaths in diabetic patients are due to vascular diseases. An ideal treatment for diabetes would be a drug that not only controls the glycemic level but also prevent the development of arteriosclerosis and other complication of diabetes.
Cardiovascular disease is one of the leading causes of death in the western world and diabetes mellitus has been identified as a primary risk factor [3], due to which there is alteration in vascular responsiveness to several vasoconstrictors and vasodilators [4]. Hypertension, a component of metabolic/insulin resistance syndrome, is an important risk factor for cardiovascular disease contributing to the increased morbidity and mortality. Oxidative stress and glucose has emerged as an important pathogenic factor in the development of hypertension.
Reactive oxygen species may contribute to the events of atherogenesis and leading to the progression of atherogenic lesions by promoting oxidation of low density lipoproteins [5]. Isoproterenol has been found to cause a severe stress in the myocardium resulting in infarct like necrosis of heart muscles. It also increases the level of serum and myocardial lipids [6] and also increases the level of cholesterol in the tissues which in turn leads to coronary heart disease [7].
Long before the use of insulin became common, indigenous remedies were used for the treatment of diabetes mellitus and hyperlipidemia. There has been an increasing demand from patients for the use of natural products with antidiabetic and antihyperlipidemia and impairment of hepatic and other body functions. The undesirable side effect and contraindications of synthetic drugs, and the fact that they are not suitable for use during pregnancy, have made scientists look towards hypoglycemia agents of plant origin. Many herb antihyperglycemia and antihyperlipidemia actions.
Hesperidin (HES) is an abundant and inexpensive byproduct of Citrus cultivation and isolated from the ordinary orange Citrus aurantium and other species of the genus Citrus (family: Rutaceae). It is reported to have anti-allergic, radio protective, immunomodulator, anti-hypertensive and antioxidant properties. When Hesperidin is administered orally, it is hydrolyzed by intestinal micro flora to yield a major active metabolite Hesperidin.
Literature survey showed that, there was no report regarding the effect of HES on glucose, HbA1c, lipid parameter and lipid metabolizing enzymes in isoproterenol induced myocardial infarction in normal and Streptozotocin-Nicotinamide induced in diabetic rats. Hence, the purpose of the present study was to instigate the effect Hesperidin on serum glucose, HbA1c, lipid parameter and lipid metabolizing enzymes in isoproterenol induced myocardial infarction in normal and Streptozotocin- Nicotinamide induced in diabetic rats.
Materials and Method
Drugs and Chemicals
Hesperidin was obtained from ACROS Lab, US. STZ and NIC were obtained from SIGMA, St. Louis, MO, USA. All other chemicals and reagents used in the study were of analytical grade.
Experimental Animals
All experiments and protocols described in present study were approved by the Institutional Animal Ethics Committee (IAEC) of Dharmaj Degree Pharmacy College, Anand. Sprague Dawley rats (205 ± 15 g) were housed in-group of 3 animals per cage and maintained under standardized laboratory conditions (12- h light/dark cycle, 24°C) and provided free access to palleted CHAKKAN diet (Nav Maharashtra Oil Mills Pvt., Pune) and purified drinking water ad libitium.
Experimental Induction of Type 2 Diabetes in Rats
Type 2 Diabetes was induced in rats by a single intraperitoneal (i.p) injection of Streptozotocin (65 mg/kg, STZ) in overnight fasting rats or mice followed by the i.p administration of Nicotinamide (110 mg/kg, NIC) after 15 minutes. STZ was dissolved in citrate buffer (pH 4.5) and NIC was dissolved in normal saline. After 7 days following STZ and NIC administration, blood was collected from retro-orbital puncture and serum samples were analyzed for blood glucose [8]. Animals showing fasting blood glucose higher than 300 mg/dL were considered as diabetic and used for the further study.
Experimental Protocol
Animals were divided into following groups, each group containing 6 animals and the treatment period for whole study was 4 weeks.
Group 1: Non-diabetic control [0.5% Sodium CMC (1 ml/kg/day, p.o) as vehicle for 4 weeks and (ND-CON)] and normal saline subcutaneously on 29th and 30th day.
Group 2: Non-diabetic control treated with HES (100 mg/kg/day, p.o) as a suspension [0.5% Sodium CMC for 4 weeks (NDHES)] and normal saline subcutaneously on 29th and 30th day.
Group 3: STZ-NIC diabetic control [0.5% Sodium CMC (1 ml/kg/day, p.o) as vehicle for 4 weeks (D-CON)] and received ISO (200mg/kg, s.c.) on 29th and 30th day in normal saline.
Group 4: STZ-NIC diabetic rats treated with HES (100 mg/kg/day, p.o) as a suspension [0.5% Sodium CMC for 4 weeks (D-HES)] and received ISO (200mg/kg, s.c.) on 29th and 30th day in normal saline.
Biochemical Estimations
Characterization of Type 2 Diabetes Model
Type 2 diabetes was confirmed by measuring fasting serum glucose using standard diagnostic kit (SPAN diagnostics Pvt., India) and the degree of uncontrolled diabetic state was confirmed by measuring HbA1c (Ion Exchange Resin method). After 4 weeks, diabetes was confirmed by measuring glucose and HbA1c as mentioned above.
Estimation of Serum Markers
On 4th week blood samples were collected from retro-orbital plexus under light ether anesthesia and centrifuged at 2500 rpm for 20 minutes to separate serum. Glucose, HbA1c, TC, TG, HDL and LDL were estimated using diagnostic kits (SPAN Diagnostics Pvt. India). The activities of lipid metabolizing enzymes such as cholesterol ester synthetase (CES), lecithin: Cholesterol acyl transferase (LCAT) and lipoprotein lipase (LPL) were determined from the heart tissues sample as suggested by Kothari et al [9], Hitz et al [10] and Slater et al [11].
Measurement of systolic and diastolic blood pressure
Systolic and diastolic blood pressure was measured indirectly in a conscious, pre-warmed, and slightly restrained rat by tail cuff method (Harvard rat-tail blood pressure monitor, USA). An average of eight consecutive reading was noted after completion of myocardial infarction in normal and STZ-NIC induced diabetic rats.
Statistical Analysis
All of the data are expressed as mean ± SEM. Statistical significance between more than two groups was tested using one-way ANOVA followed by the Bonferroni multiple comparisons test or unpaired two-tailed student’s t-test as appropriate using a computer-based fitting program (Prism, Graphpad 5). Differences were considered to be statistically significant when p<0.05.
Results
Characterization of Type 2 Diabetes
Single intraperitoneal (i.p) injection of Streptozotocin (65 mg/kg) followed by i.p administration of Nicotinamide (1100 mg/kg) to rats produced severe hyperglycemia and increased HbAIc in 70 to 80% the animals.
Effect of Hes on Serum Enzymes
There was a significant (p<0.001) increase in blood glucose and HbA1c level of STZ-NIC injected animals compared to ND-CON group (Fig. 1). Serum total cholesterol, LDL and triglyceride were significant (p<0.001) increase in STZ-NIC diabetic rats as compared to non-diabetic rats. Administration of HES in STZ-NIC diabetic rats (D-HES) significant (p<0.05) decrease on blood glucose and HbA1c, while it significantly significant (p<0.01) reduced serum total cholesterol, triglyceride and LDL (p< 0.01) in D-HES group as compared to D-CON group but there was no significant changes in the levels of HDL (Fig. 2).
Effect of HES on Lipid Metabolizing Enzymes enzyme
There was a significant (p<0.001) increase in CES after myocardial infarction in D-CON group as compared to ND-CON group (Fig. 3). Treatment of HES significant (p<0.05) decrease levels of CES as compared to diabetic rats. There was a significant (p<0.001, p<0.001) increase in LCAT and LPL after myocardial infarction in D-CON group as compared to respective ND-CON group (Fig. 3). Treatment of HES and NOB in diabetic rats significant (p<0.05) decrease levels of LCAT and LPL.
Effect of Hesperidin on systolic and diastolic blood pressure
There was a significant (p<0.01) increase in systolic and diastolic blood pressure after myocardial infarction in D-CON group as compared to ND-CON group (Fig. 4). Treatment of HES in STZ-NIC diabetic rats (D-HES) significant (p<0.05) decrease levels of systolic and diastolic blood pressure as compared to diabetic control (Fig. 4).
Discussion
The present study was under taken with the objective of exploring the Hesperidin on lipid profile, diabetic marker and Lipid Metabolizing Enzymes experimentally induced myocardial infarction in diabetic rats.
Diabetes mellitus is a chronic disorder caused by partial or complete insulin deficiency, which produces inadequate glucose control and leads to chronic complication. Premature and extensive arteriosclerosis involving renal, peripheral, and cardiovascular vessels remain the major complication of diabetes mellitus. Alteration in the serum lipid profile is known to occur in diabetes and this is likely to increase the risk for coronary heart disease. A reduction in serum lipids, particularly of the LDL and VLDL fraction and TG, should be considered as being beneficial for the long term prognosis of these patients. Lower of blood glucose and plasma lipid levels thought dietary modification and drug therapy seem to be associated with a decrease in the risk of vascular disease.
Recent studies have suggested that prevalence of type 2 diabetes is rapidly increasing. Patients with diabetes show an increased mortality concerning cardiovascular events. They more often suffer from myocardial infarction as non-diabetics mostly with a more serious course. Moreover, the post-infarction course is affected with a worse prognosis as in nondiabetics [12].
In the present study, an increase in the levels of serum glucose and HbA1c in STZ-NIC treated rats confirmed the induction of diabetes mellitus. Significant decrease was observed in the glucose and HbA1c level in diabetic rats after treatment with HES (100 mg/kg) when compared with D-CON rats at the end of experimental period. STZ causes diabetes by the rapid depletion of β-cells and thereby brings about a reduction in insulin release. HbA1c level has been reported to be increased in patients with diabetes mellitus [13]. It was reported that during diabetes mellitus, the excess of glucose present in the blood reacts with hemoglobin to form HbA1c [14]. The level of HbA1c is always monitered as a reliable index of glycemic control in diabetes [15]. Elevated levels of HbA1c observed in our study reveal that diabetes animals had prior high blood glucose level.
Lipids play an important role in cardiovascular disease, by modifying the composition, structure and stability of cell membranes. Altered lipid metabolism is considered to accelerate the development of atherosclerosis, a major risk factor in myocardial infarction. High levels of circulating cholesterol and its accumulation in heart tissue is well associated with cardiovascular damage [11]. In the present study there was a significant decrease in cardiac LCAT and LPL activity whereas a significant increase in the activity of CES was found in ISO intoxicated rats. HDL is the main substrate for LCAT for cholesterol esterification and incorporation [16].
Hypertension is a risk factor for the development and worsening of many diabetes complications, and likewise having diabetes increases your risk of developing high blood pressure. The risk of a recurrent myocardial infarction decreases with strict blood pressure. In the present study there was a significant increase in systolic and diastolic blood pressure activity in ISO intoxicated diabetic rats compared to control diabetic rats. Treatment with HES was significantly decreased in systolic and diastolic blood pressure activity in experimentally induced myocardial infarction in diabetic rats as compared to control diabetic rats.
A significant increase in the level of LCAT in diabetic rats treated with HES. In the present study hypertriglyceridemia observed in ISO intoxicated rats is due to decrease activity of LPL in the myocardium tissues. Accumulation of ester cholesterol occurs when the rate of esterification by cholesterol ester synthetase exceeds the rate of hydrolysis, which in turn results in myocardial membrane damage [17]. HES alter the activities of LCAT, LPL and CES near to the Almost normal, indicating the potential lipid lowering effects of HES.
The chronic diabetic state was also associated with dyslipedemia. This study concluded that HES at 100 mg/kg may show some protection on glucose, HbA1c and more decreased lipid profile, systolic and diastolic blood pressure and lipid metabolizing enzymes in experimentally induced myocardial infarction in diabetic rats. We concluded Hesperidin reduce cardiac complication in experimentally induced myocardial infarction in diabetic rats.
References
- Kahn SE, Porte DJ. The pathophysiology of type II (noninsulindependent) diabetes mellitus: Implications for treatment. In: Rifkin H, Porte DJ, eds. Ellenberg and Rijkin’s Diabetes Mellitus: Theory and Practice. New York: Elsevier Science 1990:436-456.
- Leibowitz HE. Oral hypoglycemic agents. In: Rifkin H, Porte DJ, eds. Ellenberg nd Rijkin’s Diabetes Mellitus: Theory and Practice. New York: Elsevier Science 1990:554-574.
- Uemura S, Matsushita H, Li W, et al. Diabetes mellitus enhances vascular matrix metalloproteinase activity: role of oxidative stress. Circ Res 2001; 88:1291-8.
- Senses V, Ozyazgan S, Ince E, et al. Effect of 5-aminoimidazole-4-carboxamide riboside (AICA-r) on isolated thoracic aorta responses in streptozotocin- diabetic rats. J Basic Clin Physiol Pharmacol 2001; 12:227– 48.
- Benelli R,Vene R, Bisacchi D, et al. Anti-invasive effects of green tea polyphenol epigallocatechin-3-gallate, a natural inhibitor of metallo and serine prostate. Biol Chem. 2002; 382: 101–105.
- Prince PS, Rajadurani M. Preventive effect of Aegle marmelos leaf extract on isoproterenol- induced myocardial infarction in rats- Biochemical evidence. J Pharm Pharmacol. 2005; 57: 1353–1357.
- Sathish V, Ebenezar KK, Devika T. Biochemical changes on the cardioprotective effect of nicorandil and amlodipin during experimental myocardial infarction in rats. Pharmacol Res. 2003; 48: 565–570.
- Masiello, P., Broca, C., Gross, R., et al. Experimental NIDDM: development of a new model in adult rats administered Streptozotocin and Nicotinamide. Diabetes 1998; 47, 224–229.
- Kothari HV, Miller BF, Kritchevsky D. Aortic cholesterol esterase: characteristics of normal rat and rabbit enzyme. Biochem Biophys Acta. 1973; 296: 446–454.
- Hitz J, Steinmetz J, Siest G. Plasma lecithin: cholesterol acyl transferase- referance values and effects of xenobiotics. Clin Chim Acta. 1983; 133: 85–96.
- Slater AM, White DA. Effect of dietary fat on cholesterol metabolism: regulation of plasma LDL concentrations. Nutr Res. 1996; 9: 241–257.
- Abel ED. Myocardial insulin resistance and cardiac complications of diabetes. Curr Drug Targets Immune Endocr Metabol Disord Jun 2005; 5(2):219-26.
- Paulsen, E.P. Heamoglobin A1C in childhood of diabetes. Metabolism 1973; 22: 269- 271.
- Koening, R.L., Peterson, C.M. Jones, R.L., et al. Correlation of glucose regulation and hemoglobin A1C in diabetes mellitus. New England Journal of Medicine 1976; 295: 417-420.
- Gabbay, K.H. Glycosylated hemoglobin and diabetic control. New England Journal Medicine 1976; 95: 443-454.
- Nestel PJ, Havel RJ, Bezman A. Metabolism of constituent lipids of dog chylomicrons. J Clin Invest. 1963; 42: 1313–1321.
- Upaganlawar A, Gandhi C, Balaraman R. Effect of green tea and vitamin E combination on isoproterenol induced myocardial infarction in rats. Plant Foods Human Nutri. 2009; 64: 75–80.