Prevalence of potentially inappropriate medications and prescription cost analysis among older cardiac patients in an outpatient department of a tertiary care hospital in India
- *Corresponding Author:
- Dr. Harsh Manishbhai Joshi
24, Jagat Janani Society, Behind Polytechnic, Ambavadi, Ahmedabad - 380 015, Gujarat, India.
E-mail: drharshmjoshi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Aims: The aim of this study is to evaluate potentially inappropriate medications (PIMs) in the elderly at cardiology outpatient department (OPD) of a tertiary care teaching hospital using Beers criteria and to find the direct cost burden of PIMs. Materials and Methods: The present study was an observational cross‑sectional study. Prescriptions of the patients’ aged ≥65 years were collected from the cardiology OPD and were analyzed. PIMs were identified with the help of Beers 2012 criteria. Direct costs of prescribed drugs were calculated. Predictors (comorbid conditions, number of drugs prescribed) associated with PIM use were identified using bivariate analysis. Multivariate logistic regression was then applied to study the influence of these variables on PIM use. A P < 0.05 was considered statistically significant. Results: A total of 236 patients received 1443 drugs. According to Beers 2012 criteria, 29.3% patients received at least one PIM followed by two and three PIMs in 10 and 23 patients, respectively. The most commonly prescribed PIM was spironolactone in 15.7% patients followed by benzodiazepines in 15 patients. The total cost of therapy for 1 day was Indian Rupee (INR) 10,029.2 while total cost of all prescribed medications in per day was INR 42.5. Conclusions: This study showed higher use of PIMs among the elderly in cardiac OPD. It is important to improve the situation of older cardiac patients who have higher use of PIMs. In older patients, high prevalence of PIMs was associated with increased cost. The use of regular continuing medical education program by the hospital and educating and training doctors on rational prescribing will help alleviate this issue.
Keywords
Aged, Beers criteria, cardiology, direct cost, potentially inappropriate medication
Introduction
Population aging is taking place in nearly all the countries of the world. The global share of older people (aged 60 years or over) increased from about 9% in 1990 to about 12% in 2013 and expected to reach about 21% by 2050, indicating high growth of elderly population in the world. As per current scenario, about 66% of the world’s older people live in developing countries.[1] In the next 40 years, elderly population in India aged 60 years and above will increase dramatically from 8% in 2010 to 19% in 2050, according to the United Nations Population Division.[2] By the year 2050, people more than 60 years of age are expected to rise to 323 million, which is higher than the population of the United States in 2012.[2]
Increasing awareness, better health care, and improving living conditions have led to increase life expectancy in geriatric population. India is considered as “an aging nation” in which 7.7% of its total population are more than 60 years of age.[3] The older people population is the highest consumer of drugs because of their various comorbidities. This leads to higher chances of polypharmacy and inappropriate medication use. Therefore, greater caution is needed while prescribing the dose, frequency, and duration of the drugs in this vulnerable group.
Potentially inappropriate medication (PIM) is defined as “a drug in which the risk of an adverse event outweighs its clinical benefit, particularly when there is a safer or more effective alternate therapy for the same condition” is available.[4] Increased incidence of adverse drug reactions (ADRs) due to PIMs has been observed by Gallagher and O’Mahony.[5] So that, it is very important to identify PIMs and minimize the drug therapy‑related adverse events in the geriatric population.
In the literature, there are various criteria for identifying PIMs, Beers criteria is one of them.[6] A geriatrician, Mark H. Beers, created the Beers criteria in 1991. These criteria were first published in the archives of internal medicine in 1991which was further updated in 1997, 2003, 2012, and 2015.[7]
Experts in the field of geriatrics, psychopharmacology, and pharmacology further modified the Beers criteria. Due to advances in pharmacology, new drugs are continually marketed while some drugs are withdrawn; hence, frequent update of such tools is required. Therefore, in 2012 and 2015, the American Geriatrics Society updated the Beers criteria using an evidence‑based approach. While the drugs on the Beer lists may cause side effects in some older adults, they will not necessarily cause these problems in all older people. Hence, one need to find out whether the side effects were actually resulted because of listed drugs taken by these patients.
In developing country like India, cardiovascular diseases such as hypertension, angina, and heart failure are common causes of morbidity and mortality. Between 2005 and 2015, India lost USD 236.6 billion because of cardiovascular diseases, stroke, and diabetes which is about 1% of the gross domestic product 10.[7] According to the year 2000 estimate, 9.2 billion productive years of life were lost among Indian adults secondary to cardiovascular disease further worsening the economic decline. As this rate rises, this estimate will increase by 2030.[8]
A careful search of the available literature resulted in no previous report of PIMs in cardiology outpatient department (OPD) and its burden of direct cost to the patients. This current study was carried out to detect PIMs focusing on cardiovascular drugs along with the direct cost of therapy in older people (>65 years) attending cardiology OPD of a tertiary care teaching hospital in India.
Materials and Methods
An observational cross‑sectional study was conducted in cardiology OPD of a tertiary care teaching hospital in Ahmedabad, Gujarat, India, after obtaining approval of the Institutional Ethics Committee (IEC). Patients aged 65 years and above were included in the study after taking their written consent. Patients who visited the cardiology OPD from February 2015 to July 2015 were included. Data were collected in a predefined case record form that included the patients’ demographic characteristics, complete medical history, clinical data, and the drugs prescribed. The Beers 2012 criteria was used to identify and assess the inappropriate prescribing.[6] We had included patients with various cardiovascular diseases as depicted in Appendix 1. Older (>65 years) cardiovascular patients may suffer from more than one disease condition at a time and tend to receive polypharmacy.
Statistical analysis
All the data were recorded in Microsoft Excel‑2010 spreadsheet. Data were analyzed using Statistical Package for Social Sciences (SPSS) software version 21 (IBM, Armonk, New York, United States). Association between polypharmacy and PIM use was determined using the Chi‑square test. Predictors (comorbid conditions, number of drugs prescribed) associated with PIM use were identified using bivariate analysis (independent variables). Multivariate logistic regression was then applied to study data. P <0.05 was considered statistically significant. Number of drugs, number of PIMs, and cost of therapy were analyzed by Pearson’s coefficient to find out linear relationship between variables. Direct costs of prescribed drugs were calculated using Indian Drug Review 2014 and current index of medical specialty online. The costs were calculated in Indian Rupee (INR).
Results
A total of 236 patients aged 65 years and above were enrolled in this study. The mean age was 68.9 ± 7.1 years and distribution of the patients according to their age groups is presented in Table 1. Within the age group of 65–70 and 81–85 years, mean numbers of drugs prescribed were 5.97 ± 0.9 and 7.4 ± 0.5, respectively; this difference in mean numbers of drugs was not statistically significant. There was statistically significant difference between mean number of drugs among 65–70 years of age group and age group of 85 years and above using unpaired t‑test (P < 0.05). No statistically significant difference was found between mean numbers of drugs in other age groups using unpaired t‑test.
| Age group | Number of | Percentage | Total number | Mean number |
|---|---|---|---|---|
| patients | of drugs | of drugs | ||
| 65-70 | 191 | 81.0 | 1141 | 5.97±0.9 |
| 71-75 | 27 | 11.4 | 174 | 6.44±1.9 |
| 76-80 | 12 | 5.1 | 81 | 6.75±0.8 |
| 81-85 | 5 | 1.7 | 37 | 7.4±0.5 |
| >85 | 2 | 0.8 | 4 | 2±0.1 |
| Total | 236 | 100 | 1437 |
Table 1: Age group pattern among patients (n=236).
A total of 236 patients were enrolled, of which 140 (59.32%) were females and 96 (40.68%) were males. The mean number of drugs prescribed in female and male group was 5.35 ± 1.9 and 7.15 ± 1.5 drugs, respectively.
Several comorbidities were analyzed in patients, of which diabetes mellitus (30.1%) was the most common followed by insomnia (6.4%), osteoarthritis (5.5%), neuropathy (5%), and chronic obstructive pulmonary disease (COPD) (2.5%).
A total of 1443 drugs were prescribed with an average of 6.11 ± 4.3 drugs per patient. Of 236 patients, 220 (93.2%) were prescribed four or more than four drugs. Between 1 and 3 drugs were administered in 16 (6.7%) patients followed by 4–6 drugs in 121 (51.2%), 7–9 drugs in 87 (36.9%), and ≥10 drugs in 12 (5.1%) patients.
Of total 236 patients, antiplatelet drug (aspirin) was the most common drug prescribed (52.5%) followed by atorvastatin (49.1%), clopidogrel (43.2%), isosorbide dinitrate (38.1%), metoprolol (30.1%), telmisartan (25%), losartan (22%), amlodipine (21.2%), ramipril (20.8%), rosuvastatin (19.5%), and furosemide (18.2%). Other less commonly prescribed drugs were metformin (11.9%), olmesartan (11.4%), and carvedilol (10.2%). Atenolol, voglibose, digoxin, multivitamins, Glyceryl trinitrate, insulin, enalapril, etc., were also prescribed to <10% patients individually. The most common combinations of drugs prescribed to the patients were clopidogrel + aspirin in 55 (23.3%) patients followed by aspirin + atorvastatin in 35 (14.8%). Antihypertensive drug combination, i.e., telmisartan + amlodipine was administered to 20 patients. Montelukast + doxofylline (sustained release) was prescribed to four patients suffering from COPD. Multivitamin tablets either alone or in combination with iron were administered to ten patients.
Paracetamol was the most prescribed nonsteroidal anti‑inflammatory drug (NSAID) (10% patients) followed by other NSAIDs such as ibuprofen (5%). For insomnia, zolpidem and lorazepam were prescribed to one and three patients, respectively. Anticoagulant drug (warfarin) was an additional drug given to ten patients along with antiplatelet. Only one antibiotic (azithromycin) was prescribed to five patients for cough. These drugs cannot be considered PIMs according to the Beers 2012 criteria. The number of drugs was positively correlated with number of PIMs (r = 0.32, P = 0.00), which was significant.
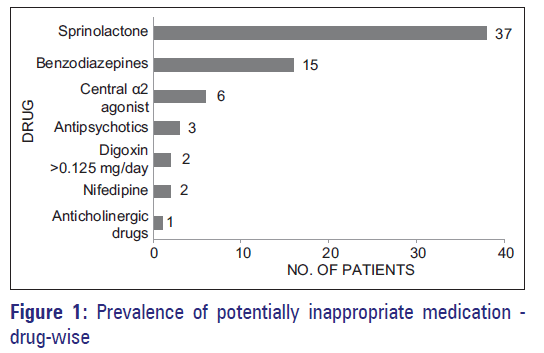
The most commonly found PIM was spironolactone in 37 (15.7%) patients followed by benzodiazepines in 15 (6.4%) patients. Other PIMs are shown in Figure 1. According to the conditions, total 61 (25.8%) PIMs were identified. Among them, NSAIDs were used in 57 (24.2%) heart failure patients followed by pioglitazone in 4 (1.7%) heart failure patients. The reasons for drugs being considered PIMs are shown in Table 2.
| PIMs | Reason |
|---|---|
| Spironolactone | Risk of hyperkalemia is higher among |
| (>25 mg/day) | older adults, especially if taking >25 |
| mg/day | |
| Benzodiazepines | Older adults have increased sensitivity to |
| benzodiazepine and slower metabolism | |
| of long-acting agents. In general, all | |
| benzodiazepines increase risk of cognitive | |
| impairment, delirium, falls, fractures, and | |
| motor vehicle accidents in older adults | |
| Central alpha 2 agonist | High risk of adverse CNS effects may |
| cause bradycardia and orthostatic | |
| hypotension, not recommended as routine | |
| treatment of hypertension | |
| Antipsychotics | Increased risk of cerebrovascular |
| accidents (stroke) and mortality in | |
| persons with dementia | |
| Digoxin (>0.125 mg/day) | In heart failure, higher dosage is |
| associated with no additional benefit | |
| and increases risk of toxicities, and slow | |
| renal clearance may cause toxicities | |
| Nifedipine | Potential for hypotension, risk of |
| precipitating myocardial ischemia | |
| Anticholinergic drugs | Avoid because of adverse CNS effects |
PIMs:Potentiallyinappropriatemedications,CNS:Centralnervoussystem
Table 2: Reasons for considering these drugs as potentially inappropriate medications.
Table 3 shows various common PIMs depicted with dose and combination whereas Table 4 shows various patterns of PIM use. The results also revealed that most of the patients (60.8%) were of 65–69 years of age group. Various PIMs in context of the disease conditions are shown in Table 4.
| Drug combinations of PIMs | Number of patients (36) | Percentage |
|---|---|---|
| Spironolactone >25 | 3 | 8.3 |
| mg/day + ACEI | ||
| Spironolactone >25 | 4 | 11.1 |
| mg/day + NSAID | ||
| Spironolactone >25 | 3 | 8.3 |
| mg/day + ARB | ||
| Aspirin + clopidogrel | 3 | 8.3 |
| Spironolactone >25 | 6 | 16.7 |
| mg/day + NSAID, ACEI | ||
| Spironolactone >25 | 17 | 47.2 |
| mg/day + NSAID, ARB |
Table 3: Various drug combinations used as potentially inappropriate medications (n=36)
| Characteristics Groups | Number of Percentage patients | ||
|---|---|---|---|
| Age | 65-69 | 42 | 60.86 |
| 70-79 | 21 | 30.43 | |
| 80-89 | 5 | 7.24 | |
| =90 | 1 | 1.44 | |
| Diagnosis | Angina pectoris | 55 | 79.71 |
| Hypertension | 45 | 65.21 | |
| Diabetes mellitus | 25 | 36.23 | |
| Heart failure | 34 | 49.27 | |
| Rheumatic heart disease | 4 | 5.79 | |
| COPD# | 4 | 5.79 | |
#COPD: Chronic obstructive pulmonary disease
Table 4:Pattern of use and patient characteristics with potentially inappropriate medications (n=69)
Significant association was found between use of PIMs and number of drugs (polypharmacy) prescribed to patients (P < 0.01). Bivariate analysis identified age of 65–70 years (odds ratio [OR]: 2.241; 95% confidence interval [95% CI]: 1.06–3.10; P = 0.009) and increased number of medications use (6–10) (OR: 0.345; 95% CI: 0.03–0.35; P < 0.05) as positive predictors of PIMs according to the Beers 2012 criteria. Gender, age, and comorbid conditions did not predict PIM use. Multivariate logistic regression analysis suggested number of drugs as positive predictor for PIM use (OR: 3.67; P < 0.01 and OR: 9.65; P < 0.001, respectively). Other predictors using multivariate logistic regression analysis showed no statistical significance.
Total cost of therapy for 236 patients for 1 day was INR 10,029.2 while average total cost of prescribed medications per day was INR 42.5. Total mean cost per month of all 236 patients was INR 297,975.1 while mean cost per patient per month was INR 1262.6. Mean cost of therapy per day in patients having PIMs was INR 62.9, which was statistically significant (P < 0.01) as compared to other patients. Of all drugs prescribed, around 5.3% drugs were administered parenterally and they were responsible for 10.1% cost burden of total cost of therapy. The contribution of antihypertensive and antiplatelet drugs to total cost of drug therapy was 29.5% and 38.6%, respectively. The number of drugs was positively correlated with cost of drug therapy (Pearson’s coefficient r = 0.5, P = 0.45), which was not statistically significant. The number of PIMs was positively correlated with cost per day (r = 0.85, P = 0.00).
Discussion
Globally, the number of the people above 65 years is on the rise due to increased life expectancy. The Beers criteria evaluates inappropriate medication use in patients of > 65 years and is one of the widely used criteria for identifying PIMs. It has undergone major changes in 2012 compared to its previous version of 2003[9] and is expected to be more competent in identifying PIMs.
Some drugs such as mesoridazine, guanadrel, ferrous sulfate, and others that are no longer in use have been omitted in the Beers 2012 criteria whereas others such as some anti‑arrhythmic drugs and belladonna derivatives that are widely prescribed have been added. Out of various categories of PIMs in Beers 2012 criteria, cardiovascular drugs are the major group where the PIMs are subdivided into therapeutic categories.
In our study, the results showed that 92.4% of patients were aged 65–75 years old; this is higher than the study conducted in Nigeria[10] where 61.8% patients were from 65 to 74 years of age group category. In the same study, it was revealed that 30.5% and 7.7% were in the 74–85 years and above 85 years of age group, respectively, which were higher than our study. Gender‑wise distribution showed that females (59.3%) were more than males in our study which is similar to other studies conducted in Europe and the USA.[11,12] Females have higher life expectancy than males in many countries[13] and this could be the reason for higher numbers of females in our study. However, this observation is inconsistent among older population in few other countries including India where male population is predominant in this age group.[14,15] The mean age in our study (69.8 ± 5.9 years) was lower than that was observed in other studies conducted among older people.[16]
In our study, various cardiovascular diseases were noted in 83.1% and 75.9% patients with angina and hypertension, respectively. An Indian study also revealed that hypertension as the major cause of morbidity affects 45% patients.[17] In our study, the prescription with the highest number of drugs per patient was 11, much lower than the studies reporting 17 and 25 drugs per prescription per patient.[18,19]
More number of drugs per prescription may lead to drug‑drug interactions, ADRs, and increased cost of therapy. In our study, the prescription pattern among geriatric population showed that antihypertensives were used in 75.9% of all prescriptions. In a study by Zaveri et al., antihypertensives were prescribed in 40.3% patients.[20] This difference may be due to the fact that this study was conducted in cardiology OPD while a study by Zaveri et al.[20] was conducted in medicine OPD.
In our study, antiplatelet drug aspirin was the most common drug prescribed (52.5%). To prevent various cardiovascular complications, aspirin (75 mg) was prescribed in 52.5% patients. This finding is consistent with the study by Christian et al.[21] where 85.6% patients received aspirin. In the study by Christian et al.,[21] 85.3% patients received clopidogrel which is higher than our study (43.2%). In our study, 83.1% patients suffered from angina pectoris, for whom antiplatelet drugs were most commonly prescribed.
The majority of patients in our study has angina pectoris (83.1%) and hypertension (75.9%) and this could be the reason that they were on drugs such as isosorbide dinitrate (38.1%) and metoprolol (30.9%). Lipid‑lowering agents such as statins were the part of medication therapy in 70% patients which is consistent with the findings of one study carried out in India.[21] Among antihypertensives, angiotensin receptor blockers (ARBs) (47%) and calcium channel blockers (CCBs) (21.2%) were the most prescribed to the patients, a finding consistent with a Nigerian study carried out on drug use in hypertension in which diuretics (84%), CCBs (66%), and angiotensin‑converting enzyme inhibitors (ACEIs, 65%) were common.[22] Atenolol (beta blocker) was the most prescribed antihypertensive in an Indian study[21] and this finding is not consistent with our study. This may be due to the change in recent guidelines for treatment of hypertension according to the Eighth Joint National Committee on Hypertension in which beta blockers are the second‑line drugs.[23] Drug combinations prescribed in our study was clopidogrel + aspirin (23.3%), which is different than a study in Nigeria where nifedipine/amiloride/ hydrochlorothiazide combination (35%) was the most common.[9]
In our study, 69 (29.2%) patients had at least one PIM. This finding is consistent with the study conducted in the USA (27.5%).[24] In one study conducted in croatia,[24] lower number of patients received PIMs. This may be explained by higher utilization of computerized systems in the pharmacy. Spironolactone, benzodiazepines, clonidine (central alpha 2 agonists), NSAIDs, antipsychotics, nifedipine, and anticholinergic drugs were the common PIMs in our study. In one Turkish study, the most common PIMs were antihistamines followed by NSAIDs and benzodiazepines.[25] The narrow safety margin drug, digoxin, was prescribed in 0.8% patients in a higher dose (>0.125 mg/day), which was higher than the study conducted in the Netherlands (0.5%),[26] while none observed in one Japanese study.[27] NSAIDs reduce potassium‑conserving action of spironolactone. Competition between canrenone (an active metabolite of spironolactone) and aspirin occurs for active transport in proximal tubule of kidney. The use of spironolactone with ARBs/ACEI can cause hyperkalemia, leading to drug‑drug interaction.
Polypharmacy was the most significant predictor of PIM use. Higher incidence of PIM associated with higher number of drugs was prescribed. Prevalence of PIM was correlated with factors such as age, gender, and associated comorbidities. Polypharmacy was more common due to higher number of comorbidities in patients, which tends to result in drug‑drug interaction, ADR, and increased cost of therapy.
The mean cost of pharmacotherapy in our study was INR 1262.6 which is higher than an Indian study, in which mean cost was INR 867.84.[28] Among all drugs, 5.3% drugs were administered parenterally adding a cost burden of 10% to the patients. This finding was comparable with another Indian study.[28] The total cost of medications in all the prescriptions per day was significantly higher than a study conducted in India,[28] in which the cost was INR 867.8. As number of PIMs increased, the cost of therapy per day also increased significantly indicating higher cost burden in patients having PIMs.
Conclusion
This study showed higher use of PIMs among older patients in cardiac OPD. In the elderly, high prevalence of PIMs is often associated with increased cost. Education and training of the doctors are necessary to prescribe rationally by focusing appropriate prescribing through teaching and conducting regular continuing medical education programs. The usage of PIMs, a major public health issue, should be further evaluated in other specialties for awareness of the prescribers.
Acknowledgements
We are thankful to the Dean of Smt. NHL Municipal Medical College, Dr. Pankaj Patel, for his support and encouragement. All authors have contributed significantly and all authors are in agreement with the content of the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- World Population Ageing 2013. Published on 2013. Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf. [Last accessed on 2016 Feb 12].
- Today’s Research on Aging. Published on March 2012. Available from: http://www.prb.org/Publications/Reports/2012/india-older-population.aspx. [Last accessed on 2016 Feb 12].
- Sanjiv B, Kanchan L, Rama R, Nilanjana G, Gautam S, Kashif S. A study of morbidity profile of geriatric population in an urban community of Kishanganj, Bihar, India. Glob J Med Public Health 2014;3:1-5.
- Corsonello A, Pranno L, Garasto S, Fabietti P, Bustacchini S, Lattanzio F.Potentially inappropriate medication in elderly hospitalized patients. Drugs Aging 2009;26 Suppl 1:31-9.
- Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): Application to acutely ill elderly patients and comparison with Beers’ criteria. Age Ageing 2008;37:673-9.
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012;60:616-31.
- Shraddha C, Bani T. Prevalence of cardiovascular disease in India and its economic impact – A review. Int J Sci Res Publ 2013;3:1-5.
- Leeder S, Raymond S, Greenberg H. A Race Against Time: The Challenge of Cardiovascular Disease in Developing Economies. New York City: Columbia University; 2004.
- Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts. Arch Intern Med 2003;163:2716-24.
- Fadare JO, Agboola SM, Opeke OA, Alabi RA. Prescription pattern and prevalence of potentially inappropriate medications among elderly patients in a Nigerian rural tertiary hospital. Ther Clin Risk Manag 2013;9:115-20.
- Steinman MA, Landefeld CS, Rosenthal GE, Berthenthal D, Sen S, Kaboli PJ. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc 2006;54:1516-23.
- Gavilán Moral E, Morales Suarez-Varela MT, Hoyos Esteban JA, Pérez Suanes AM. Inappropriate multiple medication and prescribing of drugs immobile elderly patients living in the community. Aten Primaria 2006;38:476-80.
- CIA – The World Factbook. Nigeria: People and Society Washington, DC: Central Intelligence Agency; 2012. Available from: http://www.cia.gov/library/publications/the-world-factbook/geos/ni.html. [Last updated on 2013 Jan 07; Last accessed on 2016 Feb 12].
- Zhan C, Sangl J, Bierman AS, Miller MR, Friedman B, Wickizer SW, et al. Potentially inappropriate medication use in the community-dwelling elderly: Findings from the 1996 Medical Expenditure Panel Survey. JAMA 2001;286:2823-9.
- Shah RB, Gajjar BM, Desai SV. Drug utilization pattern among geriatric patients assessed with the anatomical therapeutic chemical classifiation/defied daily dose system in a rural tertiary care hospital. Int J Nutr Pharmacol Neurol Dis 2012;2:258-65.
- Saab YB, Hachem A, Sinno S, El-Moalem H. Inappropriate medication use in elderly lebanese outpatients: Prevalence and risk factors. Drugs Aging 2006;23:743-52.
- Shenoy S. Evaluation of the drug prescribing pattern in elderly patients in tertiary care hospital. Indian J Pharmacol 2006;38:90.
- Guaraldo L, Cano FG, Damasceno GS, Rozenfeld S. Inappropriate medication use among the elderly: A systematic review of administrative databases. BMC Geriatr 2011;11:79.
- Rajska-Neumann A, Wieczorowska-Tobis K. Polypharmacy and potential inappropriateness of pharmaco-logical treatment among community-dwelling elderly patients. Arch Gerontol Geriatr 2007;44 Suppl 1:303-9.
- Zaveri HG, Mansuri SM, Patel VJ. Use of potentially inappropriate medicines in elderly: A prospective study in medicine out-patient department of a tertiary care teaching hospital. Indian J Pharmacol 2010;42:95-8.
- Christian RP, Rana DA, Malhotra SD, Patel VJ. Evaluation of rationality in prescribing, adherence to treatment guidelines, and direct cost of treatment in intensive cardiac care unit: A prospective observational study. Indian J Crit Care Med 2014;18:278-84.
- Olanrewaju TO, Aderibigbe A, Busari OA, Sanya EO. Antihypertensive drug utilization and conformity to guidelines in a sub-Saharan African hypertensive population. Int J Clin Pharmacol Ther 2010;48:68-75.
- PL Detail-Document, Treatment of Hypertension: JNC 8 and More. Pharmacist’s Letter/Prescriber’s Letter. Published on February 2014. Available from: http://www.pharmacistsletter.therapeuticresearch.com/pl/ArticlePDF.aspxcs=&s=PL&DocumentFileID=0&DetailID=3002 01&SegmentID=0. [Last accessed on 2016 Feb 12].
- Vlahovic-Palcevski V, Bergman U. Quality of prescribing for the elderly in Croatia-computerized pharmacy data can be used to screen for potentially inappropriate prescribing. Eur J Clin Pharmacol 2004;60:217-20.
- Azoulay P, Akici A, Harmanc H. Drug utilization and potentially inappropriate drug use in elderly residents of a community in Istanbul, Turkey. Int J Clin Pharmacol Ther 2005;43:195-202.
- van der Hooft CS, Jong GW, Dieleman JP, Verhamme KM, van der Cammen TJ, Stricker BH, et al. Inappropriate drug prescribing in older adults: The updated 2002 Beers criteria – A population-based cohort study. Br J Clin Pharmacol 2005;60:137-44.
- Niwata S, Yamada Y, Ikegami N. Prevalence of inappropriate medication using Beers criteria in Japanese long-term care facilities. BMC Geriatr 2006;6:1.
- Patel BJ, Patel KH, Trivedi HR. Drug utilization study in intensive coronary care unit of a tertiary care teaching hospital. NJIRM 2012;3:28-33.
| Cardiovascular disease | Percentage |
|---|---|
| Angina pectoris | 83.1 |
| Hypertension | 75.9 |
| Heart failure | 25.4 |
| Rheumatic heart disease | 3.0 |
| Left ventricular failure | 1.8 |
| Arrhythmias | 1.0 |
*Appendix 1: Frequency of cardiovascular diseases among patients (n=236)