Prescribing pattern and efficacy of anti-diabetic drugs in maintaining optimal glycemic levels in diabetic patients
- *Corresponding Author:
- Dr. Akshay A. Agarwal
F1/5/4, Gyandeep Apartment, Sector - 3/4, Vashi, Navi Mumbai - 400 703, Maharashtra, India.
E-mail: drakshay90@gmail.com
Abstract
Context: Despite the availability of efficacious anti‑diabetic drugs, which act by different mechanisms to reduce the blood‑glucose, the majority of people with diabetes on anti‑diabetic drug therapy, have poor glycemic control and diabetic vascular complications. Aim and Objectives: The aim was to study the prescribing pattern and efficacy of anti‑diabetic drugs in maintaining optimal glycemic levels in diabetic patients attending tertiary care teaching hospital in Navi Mumbai. Materials and Methods: A prospective, cross‑sectional, observational survey was carried out in 100 patients of diabetes mellitus attending diabetes outpatient/medicine outpatient departments, to assess their prescribing pattern of anti‑diabetic drugs, and their blood‑glucose level was measured by Accu‑Chek Active glucometer to determine their glycemic control. Results: Average number of anti‑diabetic drugs per prescription was 1.4. Sulfonylureas were the most commonly prescribed class, but metformin (biguanide) was the commonest prescribed individual drug among oral hypoglycemic agents (OHA). Fixed dose combination of biguanide and sulfonylurea was prescribed commonly. Monotherapy dominated over polytherapy and there was a higher percentage of use of insulin in Type 2 diabetics. Only 41% of patients on anti‑diabetic therapy had optimal glycemic control. The association between anti‑diabetic therapy along with lifestyle modification and glycemic control was statistically significant (P = 0.0011). Conclusions: OHAs still dominate the prescribing pattern, but there was a shifting trend toward the use of insulin preparations in the management of Type 2 diabetes mellitus. In achieving optimal glycemic control, the efficacy of the anti‑diabetic drugs was only 41%; therefore intensification of current drug treatment as well as planning multiple drug interventions with lifestyle modification is necessary.
Key words
Anti-diabetic drugs, diabetes, glycemic control, insulin, oral hypoglycemic agents, prescribing pattern
Introduction
Diabetes mellitus is a pandemic disease that has struck each and every corner of the world. According to the Indian Council of Medical Research-Indian Diabetes study (ICMR), a national diabetes study, India currently has 62.4 million people with diabetes.[1] This is set to increase to over 100 million by 2030.[2] The prevalence of diabetes among adults has reached approximately 20% in urban and approximately 10% in rural populations in India.[3]
Various classes of anti-diabetic drugs including insulin and oral hypoglycemic agents (OHA) are currently used in the treatment of diabetes, which acts by different mechanisms to reduce the blood-glucose levels to maintain optimal glycemic control.[4,5]
The United Kingdom Prospective Diabetes Study showed intensive blood-glucose control by either sulfonylureas or insulin substantially decreased the risk of microvascular complications.[6,7]
The currently used anti-diabetic drugs are very effective, however because of lack of patient compliance, clinical inertia, insulin resistance, lack of exercise and lack of dietary control leads to unsatisfactory control of hyperglycemia.[8-15] In India, limited studies have focused on diabetes care and provide an insight into the current profile of patients and their management. More than 50% of people with diabetes have poor glycemic control, uncontrolled hypertension and dyslipidemia, and a large percentage have diabetic vascular complications.[16,17]
Therefore, this study was carried out to find the current prescribing pattern of anti-diabetic drugs and efficacy of these drugs in maintaining adequate glycemic control in diabetic patients attending a tertiary care teaching hospital in Navi Mumbai.
Materials and Methods
This was a cross-sectional, prospective, observational study carried out in Diabetology and Medicine Department of a Tertiary Care Hospital in Navi Mumbai and was conducted for the ICMR Short Term Research Studentship (2010) program. Permission from ethics committee was obtained prior to the conduct of the study. The sample size for this study was 100 patients (95% confidence interval, ±10%) in accordance with World Health Organization (WHO) manual to assess drug use in individual facilities.[18] It was a pilot study with duration of 2 months (May 10, 2010 to July 10, 2010) in which 100 patients of diabetes of 18 years and above receiving anti-diabetic therapy for more than 1 year was randomly selected for participation after fulfilling inclusion/exclusion criteria. After obtaining informed consent, sociodemographic data along with details of anti-diabetic drug therapy, duration of treatment and life style modifications (dieting/exercise/both) was recorded. In addition, fasting and postprandial blood-glucose was measured by Accu-Chek Active glucometer. We excluded newly diagnosed diabetic patients, diabetic patient on anti-diabetic therapy for <1 year, diabetic coma patients, repeat attendance, patients not willing for informed consent and blood-glucose investigation.
The following parameters were analyzed:
Average number of anti-diabetic drugs per prescription, percentage of different class of anti-diabetic drug prescribed, commonest class and type of anti-diabetic drugs prescribed, percentage of anti-diabetic drugs prescribed from essential drug list (WHO and Indian National Essential Drug List).[19,20] Patients were categorized with optimal controlled glycemic level based upon the blood-glucose level (fasting <100 mg/dL and/or postprandial <180 mg/dL) measured by Accu-Chek Active glucometer.
The study data were analyzed on the Statistical Package for the Social Sciences version 17 (Chicago: SPSS Inc), with P < 0.05 was considered to be statistically significant. Chi-square test was used for categorical data to test for the association. Data were expressed in terms of the actual number, mean, and percentages.
Results
One hundred (n = 100) patients of Type 2 diabetes were analyzed and 140 anti-diabetic drug products were prescribed. Male were 54% (n = 54), female were 46% (n = 46) and the mean age of the sample was 58.12 (±10.5) years.
Prescribing pattern
During the study, the number of anti-diabetic drug products per prescription varied from one to four and the average number of anti-diabetic drugs per prescription was 1.4.
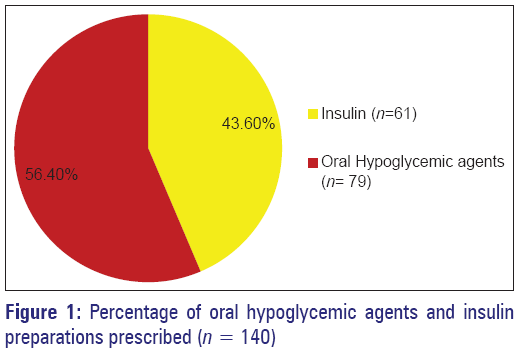
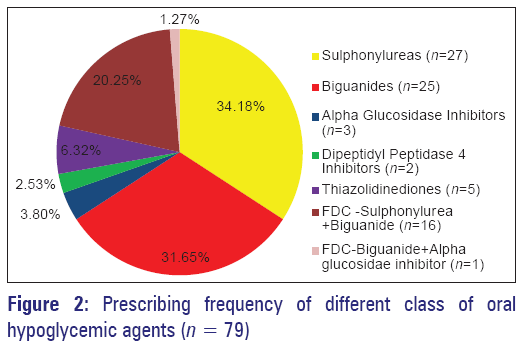
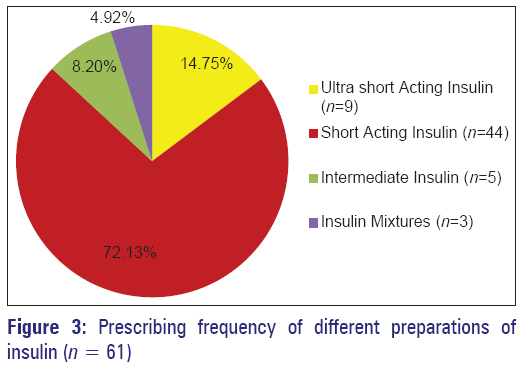
Out of total 140 prescribed anti-diabetic drug products, 79 (56.4%) were OHA and 61 (43.6%) were insulin [Figure 1]. Thus OHA’s were the most common class of anti-diabetic drugs prescribed in this study. Sulfonylureas (34.14%) were the most commonly prescribed class followed by biguanides (31.65%) among the different classes of OHA [Figure 2] and their fixed dose combination (FDC) accounted for 20.25%. Metformin (biguanide) was the most common individual OHA to be prescribed 31.65%, followed by glimepiride (sulfonylurea) 20.25%, followed by FDC of glimepiride plus metformin 11.40% [Table 1]. Other classes of OHA prescribed were thiazolidinediones 6.33%, alpha glucosidase inhibitor 3.8%, and dipeptidyl peptidase 4 inhibitors (DPP 4 inhibitors) 2.5%, respectively. Insulin preparations accounted for 43.6% of the total anti-diabetic drugs and the most common preparation was short acting insulin preparation [Figure 3].
| OHA (s) | Number (out of 79) | Percentage |
|---|---|---|
| Metformin | 25 | 31.65 |
| Glimepiride | 16 | 20.25 |
| Gliclazide | 7 | 8.86 |
| Glipizide | 2 | 2.54 |
| Glibenclamide | 2 | 2.54 |
| Acarbose | 2 | 2.54 |
| Voglibose | 1 | 1.26 |
| Pioglitazone | 5 | 6.33 |
| Sitagliptin | 1 | 1.26 |
| Saxagliptin | 1 | 1.26 |
| FDC (glimepiride+metformin) | 9 | 11.40 |
| FDC (gliclazide+metformin) | 5 | 6.33 |
| FDC (glyburide+metformin) | 1 | 1.26 |
| FDC (glipizide+metformin) | 1 | 1.26 |
| FDC (voglibose+metformin) | 1 | 1.26 |
FDC: Fixed dose combination
Table 1: Prescribing frequency of different OHAs
Brand versus generic and selection of essential drugs
All the drugs were prescribed by brand names (100%). Percentage of drugs prescribed from WHO essential drug list was 74.2% (104) and National Essential Drug List of India was 67.1% (94).
Optimal glycemic control
Of the 100 Type 2 diabetic patients who were receiving anti-diabetic drugs, 41 (41%) had controlled optimal glycemic levels, while 59 (59%) had inadequately controlled glycemic levels [Table 2]. Association between optimal glycemic levels was statistically significant in diabetic patients on anti-diabetic therapy with lifestyle modification (P = 0.0011); however, this association with type of therapy and duration of treatment was not significant statistically (P > 0.05).
| Characteristics | Glycemic level | Total | P | |
|---|---|---|---|---|
| Controlled Uncontrolled | (n=100) | |||
| Diabetic patients (Type 2) | 41 | 59 | 100 | |
| Age (years) | ||||
| <40 | 4 | 2 | 6 | 0.66 |
| 40-60 | 20 | 32 | 52 | |
| >60 | 17 | 25 | 42 | |
| Sex | ||||
| Males | 21 | 33 | 54 | 0.64 |
| Females | 20 | 26 | 46 | |
| BMI | ||||
| Normal (18.5-24.9) | 19 | 19 | 38 | 0.34 |
| Overweight (25-30) | 16 | 28 | 44 | |
| Obese (above 30) | 6 | 12 | 18 | |
| Type of anti-diabetic | ||||
| therapy | ||||
| Monotherapy | 25 | 34 | 59 | 0.73 |
| Combination therapy | 16 | 25 | 41 | |
| Duration of treatment | ||||
| (years) | ||||
| <5 | 18 | 27 | 45 | 0.96 |
| 5-10 | 16 | 23 | 39 | |
| >10 | 7 | 9 | 16 | |
| Anti-diabetic therapy | ||||
| With life style | 35 | 32 | 67 | 0.0011 |
| modifications | ||||
| Without life style | 6 | 27 | 33 | |
| modifications | ||||
BMI: Body mass index
Table 2: Characteristics of diabetic patients based on glycemic control
Discussion
In this study, an attempt has been made to describe the current prescribing pattern and trend of anti-diabetic drug therapy along with the efficacy of these drugs in maintaining an optimal glycemic level in diabetic patients in a tertiary care hospital in Navi Mumbai.
In this study, out of 100 patients who were treated with anti-diabetic drugs all of them were Type 2 diabetic patients (noninsulin dependent diabetes mellitus) that reflect the increasing prevalence of Type 2 diabetes mellitus in our region.
The average number of anti-diabetic drugs per prescription in this study was 1.4. Previous hospital based studies in India and Abroad has reported 2-5 drugs per prescription.[21-26] Our study showed restraint on polypharmacy.
In this study, OHAs were commonly prescribed drugs accounting for 56.40% of the total prescribed anti-diabetic products. Sulfonylureas (34.14%) were the most commonly prescribed class, which was similar to previous studies,[22,24,27] followed by biguanides (31.65%) and their FDC accounted for 20.25%. This reflects that sulfonylureas and biguanides are still the choice of most physicians in the treatment of Type 2 diabetes.
In spite of sulfonylurea being the commonest class, we observed that metformin (biguanide) was the most common individual OHA to be prescribed 31.65% which is similar to several studies[21,23,27-29] followed by glimepiride (sulfonylurea) 20.25%. This may be due to the fact that metformin was the only drug of its class to be prescribed, whereas many second generation sulfonylureas are available and were prescribed making their individual frequency low but as a group/class their prescribing was higher than biguanide class. The study documented low prescribing frequency of newer OHA (thiazolidinedione and DPP 4 inhibitors). They were used in combination with other OHAs in order to achieve better glycemic control which was similar to previous studies.[22,28]
Insulin preparations accounted for 43.6% of the total anti-diabetic drugs and the most common preparation was short acting insulin preparation. We found a higher percentage of insulin prescribing and insulin based therapy in our study compared with previous Indian studies.[23,24] Insulin preparations can provide intensive, near-physiologic delivery of insulin and can help patients achieve better glycemic control.[30] This reflects a change in prescribing trend and shift toward insulin based therapy from the dominated class of OHA in Type 2 diabetes treatment.
In this study, all drugs were prescribed by brand name suggesting popularity of the brands among the physician and influence of pharmaceutical companies on the physician. It is advisable to prescribe by generic name for cost effective utilization. However, in this study the percentage of drugs prescribed from national essential drug list was 67.1% which showed the awareness and selection of drugs from essential drug list for rational use of drugs.
About 41% patients on anti-diabetic drugs had controlled optimal glycemic levels, while 59% had inadequate/ uncontrolled glycemic levels. Several studies[15,31-34] have documented from 50% to 86%, which were higher than our studies. Although these variations across studies may be true, they may also be due to differences in populations surveyed, methods of data collection, measurements of blood-glucose/hemoglobin A1c (HbA1c), and definitions of blood-glucose/HbA1c cut-point for adequate glycemic control.
The most prevalent anti-diabetic therapy was monotherapy either with OHA or insulin, while combination therapy with OHA’s and insulin was to a lesser extent. Study by Willey et al.,[32] has documented good glycemic control on monotherapy. However in our study, association of glycemic control with monotherapy and combination therapy was not statistically significant (P > 0.05). However, we found a statistically significant association between glycemic control and anti-diabetic drug therapy with lifestyle modification. Thus, lifestyle modification along with anti-diabetic drug treatment has the potential to improve glycemic control in patients with Type 2 diabetes despite optimized anti-diabetic drug treatment.[6,7,35]
The study strongly highlights the domination of OHA but documents shifting trend towards insulin in the treatment of Type 2 diabetes and the need for periodic blood-glucose monitoring in patients receiving anti-diabetic drug treatment to identify inadequately controlled glycemic levels, so that drug therapy can be intensified and multiple drug interventions can be planned in order to obtain an optimal glycemic level. It also highlights the need for lifestyle modification measures along with anti-diabetic drug treatment for achieving better glycemic control in Type 2 diabetes.
Limitations of the Study
It was a pilot study of 2 months duration conducted in 100 diabetic patients. Measurement of HbA1c level, which is considered as the gold standard and gives better judgment about 3 months glycemic control, was not done due to its high cost. Measurement of blood-glucose was done with Accu-Chek Active glucometer instead of laboratory glucose oxidase-peroxidase method. Accu-Chek Active glucometer was used due to its ease of self-monitoring of blood-glucose and it correlated well with the laboratory blood-glucose values.[36]
Conclusion
Oral hypoglycemic agents still dominate the prescribing pattern, but there was a shifting trend toward the use of insulin preparations in the management of Type 2 diabetes mellitus. In achieving optimal glycemic control, the efficacy of the anti-diabetic drugs was only 41%; therefore intensification of current drug treatment as well as planning multiple drug interventions with lifestyle modification is necessary to prevent diabetic complications.
Acknowledgments
ICMR STS-2010 Program.
References
- Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia 2011;54:3022-7.
- International Diabetes Federation. IDF Diabetes Atlas. 5th ed. Brussels, Belgium: International Diabetes Federation; 2011. [Last accessed on 2012 Jul 10]. Available from: http://www.idf.org/diabetesatlas.
- Ramachandran A, Snehalatha C. Current scenario of diabetes in India. J Diabetes 2009;1:18-28.
- Davis SN. Insulin, oral hypoglycemic agents, and pharmacology of the endocrine pancreas. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman and Gilman`s The Pharmacological Basis of Therapeutics. 11th ed. United States of America McGraw-Hill; 2006. p. 1613-45.
- Powers AC. Diabetes mellitus. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Lango DL, Jameson JL, editors. Harrison`s Principles of Internal Medicine. 16th ed. New york McGraw-Hill; 2005. p. 2152-80.
- Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:854-65.
- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837-53.
- Grant R, Adams AS, Trinacty CM, Zhang F, Kleinman K, Soumerai SB, et al. Relationship between patient medication adherence and subsequent clinical inertia in type 2 diabetes glycemic management. Diabetes Care 2007;30:807-12.
- Lafata JE, Dobie EA, Divine GW, Ulcickas Yood ME, McCarthy BD. Sustained hyperglycemia among patients with diabetes: What matters when action is needed? Diabetes Care 2009;32:1447-52.
- Feldstein AC, Nichols GA, Smith DH, Rosales AG, Perrin N. Weight change and glycemic control after diagnosis of type 2 diabetes. J Gen Intern Med 2008;23:1339-45.
- Bi Y, Yan JH, Liao ZH, Li YB, Zeng LY, Tang KX, et al. Inadequate glycaemic control and antidiabetic therapy among inpatients with type 2 diabetes in Guangdong Province of China. Chin Med J (Engl) 2008;121:677-81.
- Adler AI, Shaw EJ, Stokes T, Ruiz F, Guideline Development Group. Newer agents for blood glucose control in type 2 diabetes: Summary of NICE guidance. BMJ 2009;338:b1668.
- Karter AJ, Moffet HH, Liu J, Parker MM, Ahmed AT, Go AS, et al. Glycemic response to newly initiated diabetes therapies. Am J Manag Care 2007;13:598-606.
- Yurgin N, Secnik K, Lage MJ. Antidiabetic prescriptions and glycemic control in German patients with type 2 diabetes mellitus: A retrospective database study. Clin Ther 2007;29:316-25.
- Mendes AB, Fittipaldi JA, Neves RC, Chacra AR, Moreira ED Jr. Prevalence and correlates of inadequate glycaemic control: Results from a nationwide survey in 6,671 adults with diabetes in Brazil. Acta Diabetol 2010;47:137-45.
- Raheja BS, Kapur A, Bhoraskar A, Sathe SR, Jorgensen LN, Moorthi SR, et al. DiabCare Asia – India Study: Diabetes care in India – current status. J Assoc Physicians India 2001;49:717-22.
- Nagpal J, Bhartia A. Quality of diabetes care in the middle- and high-income group populace: The Delhi Diabetes Community (DEDICOM) survey. Diabetes Care 2006;29:2341-8.
- World Health Organization (WHO) and International Network for Rational Use of Drugs. How to Investigate Drug Use in Health Facilities: Selected Drug Use indicators. Geneva, Switzerland: WHO; 1993. (WHO/DAP/93.1).
- National List of Essential Medicines of India 2011. Ministry of Health and Family Welfare, Government of India. Available from: http://www.pharmaceuticals.gov.in/NLEM.pdf. [Last cited on 2012 Jan 10].
- WHO Essential Medicine List 2011. World Health Organization. Available from: http://www.whqlibdoc.who.int/hq/2011/a95053_eng. pdf. [Last cited on 2012 Jan 10].
- Adibe MO, Aguwa CN, Ukwe CV, Okonta JM, Udeogaranya PO. Outpatient utilization of anti-diabetic drugs in the South Eastern Nigeria. Int J Drug Dev Res 2009;1:27-36.
- Hasamnis A, Patil S. Prescription pattern study in type 2 diabetes mellitus in an Indian referral hospital. Internet J Pharmacol 2009;7:1.
- Rajeshwari S, Adikhari P, Pai MR. Drug utilisation study in geriatric type 2 diabetic patients. J Clin Diagn Res 2007;1:440-3.
- Sutharson L, Hariharan RS, Vamsadhara C. Drug utilization study in diabetology outpatient setting of a tertiary hospital. Indian J Pharmacol 2003;35:237-40.
- Shamna M, Karthikeyan M. Prescription pattern of antidiabetic drugs in the outpatient departments of hospitals in Malappuram district, Kerala. J Basic Clin Physiol Pharmacol 2011;22:141-3.
- Patel B, Oza B, Patel KP, Malhotra SD, Patel VJ. Pattern of antidiabetic drugs use in type-2 diabetic patients in a medicine outpatient clinic of a tertiary care teaching hospital. Int J Basic Clin Pharmacol 2013;2:485-91.
- Truter I. An investigation into antidiabetic medication prescribing in South Africa. J Clin Pharm Ther 1998;23:417-22.
- Sultana G, Kapur P, Aqil M, Alam MS, Pillai KK. Drug utilization of oral hypoglycemic agents in a university teaching hospital in India. J Clin Pharm Ther 2010;35:267-77.
- Hassan Y, Mathialagan A, Awaisu A, Aziz NA, Yahaya R, Salhani A. Trend in the use of oral hypoglycemic agents in an outpatient pharmacy department of a tertiary hospital in Malaysia (2003-2006). Asian J Pharm Clin Res 2009;2:40-6.
- Shah S, Das AK, Kumar A, Unnikrishnan AG, Kalra S, Baruah MP, et al. Baseline characteristics of the Indian cohort from the IMPROVE study: A multinational, observational study of biphasic insulin aspart 30 treatment for type 2 diabetes. Adv Ther 2009;26:325-35.
- Patel B, Oza B, Patel KP, Malhotra SD, Patel VJ. Pattern of antidiabetic drugs use in type-2 diabetic patients in a medicine outpatient clinic of a tertiary care teaching hospital. Int J Basic Clin Pharmacol 2013;2:485-91.
- Willey CJ, Andrade SE, Cohen J, Fuller JC, Gurwitz JH. Polypharmacy with oral antidiabetic agents: An indicator of poor glycemic control. Am J Manag Care 2006;12:435-40.
- Ben Abdelaziz A, Soltane I, Gaha K, Thabet H, Tlili H, Ghannem H. Predictive factors of glycemic control in patients with type 2 diabetes mellitus in primary health care. Rev Epidemiol Sante Publique 2006;54:443-52.
- Moreira ED Jr, Neves RC, Nunes ZO, de Almeida MC, Mendes AB, Fittipaldi JA, et al. Glycemic control and its correlates in patients with diabetes in Venezuela: Results from a nationwide survey. Diabetes Res Clin Pract 2010;87:407-14.
- DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med 1999;131:281-303.
- Ullal A, Parmar GM, Chauhan PH. Comparison of glucometers used in hospitals and in outpatient settings with the laboratory reference method in a tertiary care hospital in Mumbai. Indian J Endocr Metab 2013;17:688-93.