Penile Calciphylaxis in Chronic Renal Failure Patient: A Case Study
- *Corresponding Author:
- Omar Thanoon Dawood
School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia.
E-mail: othd2000@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Penile calciphylaxis occasionally seen in chronic renal failure patients. Causes include vascular calcification in accordance with elevated levels of serum calcium and phosphorus. Worldwide very few cases have been reported and estimated nearly 4% of ESRF patients are affected. Now we are presenting a case of penile calciphylaxis in a 76-year diabetic patient with ESRF. The condition overall carries a poor prognosis. Postulated methods of treatment can be made includes primary wound care, calcium phosphate level reduction by hemodialysis and sodium thiosulfate, and parathyroid hormone level reduction
Introduction
Penile calciphylaxis occurs as a consequence of vasculopathy is seen in patients with diabetes with chronic renal failure on long term hemodialysis. [1] It also known as Calcemic Uremic Arteriolopathy (CUA). [2,3] It was first described in uremic patients by Bryant and White in 1898, though the term calciphylaxis was initially penned by Hans Seyle in 1962. [4] It is uncommonly seen but with more patients developing renal complications after diabetes and renal transplant recipients rising, the numbers are likely to rise. This case report of penile calciphlaxis can help nephrologists, surgeons, and dermatologists to recognize it well and paying more attention to such patients due to the poor prognosis of calciphylaxis that can be associated with patient’s condition.
Case Report
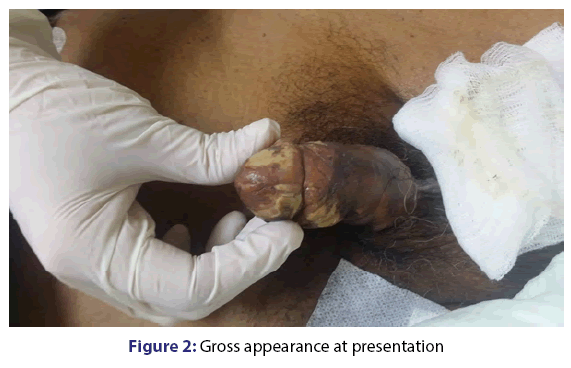
A 76-year-old, Malay gentleman with past medical history of diabetes mellitus, hypertension, ischemic heart disease (double vessel disease) ESRD on regular HD 1,3,5 for the past 6 years was admitted to the medical intensive unit for community acquired pneumonia in sepsis. The patient was unwell for the past 1/52, presented with progressive worsening shortness of breath and fever. He defaulted his regular hemodialysis for the past 2 sessions. On presentation, he was septic looking, lethargic and tachypneic with having a temperature spike of 38.6°C, blood pressure of 90/50 mmHg and pulse rate of 112 bpm. Auscultation reveals generalized crepitation. The patient was resuscitated and intubated for type 1 respiratory failure. Complete general examination was later revealed a penile ulcerous lesions and urology team was consulted. Several calcified plagues were noted with ulcer gangrenous evolution over entire penile region. No further history could be obtained as the patient lives alone [Figures 1 and 2].
Blood investigations: hemoglobin and hematocrit of 8.7 g/dl and 33.7%, white blood cell (WBC) count 23.7, platelet count 112, sodium 125 mmol/L, potassium 6.3 mmol/L, chloride 107 mmol/L, glucose 186 mg/dl, urea 45 mg/dl, creatinine 876 mg/dl, PTH level was 190 pg/ml (normal=12-64 pg/ml). Clinical diagnosis of penile calciphylaxis was made and planned for penile Doppler study and wound debridement.
Unfortunately, patient general condition worsened and passed away one day later due to sepsis with coagulopathy secondary community acquired pneumonia.
Discussion
In general from literature, penile calciphylaxis cases were associated with end stage renal failure (ESRF) and diabetic nephropathy and vasculopathy. [1] Other associated conditions predisposing to calciphylaxis are malignancy, primary hyperparathyroidism, alcoholic cirrhosis, inflammatory bowel disease, systemic lupus erythematosus (SLE), chronic myelogenous leukemia (CML), and acquired immunodeficiency syndrome (AIDS). [5]
Common clinical presentation would be white or yellowish cutaneous lesions showing a wide spectrum of involvement from small areas of livedo reticularis and single plaques to ulcerous and necrotizing lesions. Other possible areas of involvement are upper limbs, lower limbs, buttocks, thighs, and trunk. Proximal involvement associated with unfavorable prognosis. Pathogenetic pathways of penile calciphylaxis are still partially unclear. [6] As penile calciphylaxis commonly associated with ESRF patients, main risk factor for developing calciphylaxis is uremia. [7] Other factors such as raise parathyroid hormone and serum phosphate levels could be affiliated to vascular calcifications leading to penile calciphylaxis. [8] So far there have been no studies to support the role of parathyroidectomy as a modality of mainstream treatment of penile calciphylaxis, although it could relieve pain and speed up skin wounds. [9]
Close control of phosphatemia with phosphate-binding agents is crucial to prevent clinical development of penile calciphylaxis. Sodium thiosulfate has provided good result in treating calciphylaxis cutaneous wounds. Its role as a potent antioxidant has been noted to promptly decrease pain, and its chelating properties are affiliated with regression of subcutaneous calcifications. In addition, hyperbaric oxygen therapy increases oxygen delivery to tissues. By increasing oxygen supply, it promotes cutaneous lesions healing via neoangiogenesis, fibroblastic growth, and collagen expression. [10]
References
- Wilmer WA, Magro CM. Calciphylaxis: Emerging concepts in prevention, diagnosis and treatment. Seminars in Dialysis 2002;15:172-86.
- Llach F. Calcific uremic arteriolopathy (calciphylaxis): An evolving entity? Am J Kidney Dis 1998;32:514-8.
- Angelis M, Wong LL, Myers SA,Wong LM. Calciphylaxis in patients on hemodialysis: a prevalence study. Surgery 1997;122:1083-9.
- Guldbakke KK, Khachemoune A. Calciphylaxis. IntJDermatol 2007;46:231-8.
- Mathur AV, Azad S, Singh M, Anand N. Penile necrosis in association with chronic renal failure; Calciphylaxis or Calcific uremic arteriolopathy. JDiab 2013;2:5.
- Frank AG Jr. Skin manifestation of internal disease.Med Clin North Am 2009;93:1265-82.
- Weenig RH,Sewell LD,Davis MD,McCarthy JT, Pittelkow MR. Calciphylaxis: natural history, risk factor analysis and outcome.J Am Acad Dermatol 2007;56:569-79.
- Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating: risk factors, outcome and therapy.Kidney Int 2002;61:2210-7.
- Ross EA. Evolution of treatment strategies for calciphylaxis. Am JNephrol 2011;34:460-7.
- Tamura M, Hiroshige K, Osajima A, Soejima M,Takasugi M,Kuroiwa A. A dialysis patient with systemic calciphylaxis exhibiting rapidly progressive visceral ischemia and acral gangrene.Intern Med 1995;34:908-12.