Optimization of liposomal encapsulation for ceftazidime for developing a potential eye drop formulation
- *Corresponding Author:
- Dr. Marianna Budai
Department of Pharmaceutics, Semmelweis University, Högyes E. u. 7, Budapest, Hungary.
E-mail: budai.marianna@pharma.semmelweis-univ.hu
Abstract
Ceftazidime is a broad spectrum third generation cephalosporin antibiotic which is effective mainly against Gram-negative bacteria such as Pseudomonas aeruginosa, Acinetobacter and Enterobacteriaceae, the pathogens which most often cause ophthalmological infections. Unlike other commonly used beta lactam antibiotics, ceftazidime is resistant to several types of beta lactamases (e.g., TEM, SHV and PSE-1). Because of these advantages, ceftazidime is used in the treatment of eye infections. However, ceftazidime undergoes rapid degradation in aqueous solutions therefore eye drops containing ceftazidime in aqueous solutions are not commercially manufactured. In the present study, liposomal encapsulations of ceftazidime with various lipid compositions, hydrating solutions and pH-values have been studied in order to optimize liposomal composition for a potential eye drop formulation.
Keywords
Ceftazidime, encapsulation, liposome, ophthalmology
Introduction
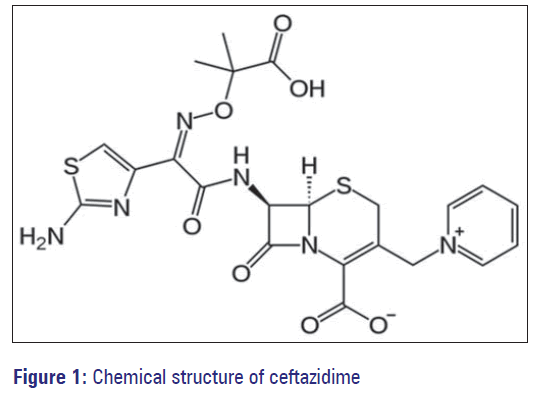
Ceftazidime is a third generation semisynthetic, broadspectrum cephalosporin antibiotic for parenteral administration. Like other third generation cephalosporins, it has a broad spectrum activity against Gram-positive and Gram-negative (e.g., Neisseria gonorrhoeae, Enterobacteriaceae, Acinetobacter) bacteria [Figure 1]. However, unlike most third-generation agents, it is active against Pseudomonas aeruginosa. Furthermore, ceftazidime is resistant to several types of beta lactamases (e.g., TEM, SHV and PSE-1). Thus, ceftazidime is usually reserved for the treatment of serious lower airway’s infections, septicemia and cerebrospinal meningitis. Ceftazidine is the first line treatment for the rare tropical infection, melioidosis. [1-3] Ceftazidime is usually given intravenous or intramuscular. Every 8-12 h (2-3 times a day), with daily dosages of 500-6,000 mg, determined by the indication, infection severity and/or renal function of the patient. Ceftazidime pentahydrate containing products are marketed under various trade names such as Cefzim® (Pharco B International), Fortum® (GSK) and Fortaz® (GSK).
Ceftazidime is also used for the treatment of ophthalmological infections caused in particular by P. aeruginosa. Pseudomonas is among the principal pathogens associated with corneal ulcers and ceftazidime is the only third generation cephalosporin with good coverage against it. [2] However, ceftazidime undergoes rapid degradation in aqueous solutions, resulting in the opening of the beta-lactam ring. The rate of degradation depends – among others - on temperature, light, composition of the solvent, pH and ceftazidime concentration. [1,4] Therefore, eye drops containing ceftazidime in aqueous solutions are not commercially manufactured.
In the present study, liposomal encapsulations of ceftazidime with various lipid compositions and hydrating solutions have been studied in order to develop novel eye drop formulations to treat ophthalmological infections.
Materials and Methods
The lipids used in these experiments were 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC) and 1,2-dipalmitoyl-sn-glycero-3-phospho-(1’-rac-glycerol) (sodium salt) (DPPG) and 1,2-di-O-octadecenyl-3- trimethylammonium propane (chloride salt) (DOTMA) from Avanti Polar Lipids Inc. (Alabaster, AL, USA). Ceftazidime and cholesterol were purchased from Sigma Aldrich (St. Louis, MO, USA). Absolute ethanol (Sigma Aldrich, St. Louis, MO, USA) was used as the solvent to dissolve the lipids. Sodium phosphate, monobasic and dibasic (J T Baker, Phillipsburg, NJ, USA) were used to prepare the buffer solutions.
Preparation of liposomes
Lipid mixtures were prepared by combining the appropriate lipids in 9:1 molar ratio (DPPC + DPPG, DPPC + DOTMA, DPPC + cholesterol).
Multilamellar vesicles were prepared using the dehydration/ rehydration method. The mixture of chloroform and ethanol (2:1 v/v) was used to dissolve the lipid mixtures. A thin lipid film was formed in a round bottom flask by evaporating the solvent from the lipid solution in a rotary evaporatior at water bath temperature of 45°C for 30 min and at the room temperature (25°C) for 20 min under constant flow of argon gas. The dry lipid films were stored in a desiccator at the room temperature.
For ceftazidime encapsulation, the antibiotic containing hydrating solution (30 mg/mL) was added at room temperature to the liposome tube in five equal aliquots to reach the final volume (1 mL). 0.1 M phosphate buffer, 0.9% saline, 5% dextrose and 10% sucrose at pH 7.4 – containing ceftazidime – were used as hydrating solutions. After the addition of hydrating solution, the round bottom flask was vortexed to ensure the homogeneity of the mixture. The final lipid concentration was 30 mg/mL in each case, resulting in about a 1.33-1 ceftazidime to lipid ratio.
Measurement of encapsulation efficiency
Freshly prepared ceftazidime-liposomes (1 mL) were centrifuged with the Galaxy 16DH eppendrof centrifuge (2 × 10 min, 13,000g) through Nanosep 10K Omega Centrifugal Filter Devices (PALL Life Science Inc.) with a cut-off value of 10 kDa to separate the liposomes from the solution.
The encapsulation efficiencies for ceftazidime were determined by spectrophotometry (Shimadzu ultravioletvisible spectrophotometer, 2101-PC) at a wavelength of 296 nm. The absorbance values of the ceftazidime containing hydrating solutions (Absi) and the absorbance of the filtered outer phase of liposomal samples (Absf) were determined.
The encapsulation efficiency was determined using the following equation:
EE = (Absi − Absf)/Absi × 100.
Results
Throughout our experiments for liposomal encapsulation, 3% ceftazidime concentrations were used. According to the literature data, 1% ceftazidime eye drops are applied in the treatment of infections of the external eye structures while 5% formulations are used in case of severe infections of front or internal eye structures. [1]
The composition of the liposome affects the amounts of ceftazidime encapsulated. Among the compositions tested throughout our study, the highest ceftazidime encapsulation − 17.72 ± 0.92% – was achieved using DPPC: DPPG combination in 9:1 molar ratio [Table 1]. The presence of the cationic lipid DOTMA decreased the ceftazidime encapsulation value (13.03 ± 2.63%). This observation can be explained with electrostatic interactions between the lipid bilayer and drug negatively influencing the rate of encapsulation. The positively charged quaternary ammonium of ceftazidime may play a significant role in the above mentioned fact.
| Lipid mixture used to prepare liposomes (9:1 molar ratio) | Encapsulation efficiency (%) of ceftazidime (±SD) |
|---|---|
| DPPC:DPPG | 17.72±0.92 |
| DPPC:DOTMA | 13.03±2.63 |
| DPPC:Cholesterol | 14.82±2.68 |
SD: Standard deviation, DPPC: 1,2-dipalmitoyl-sn-glycero-3- phosphocholine, DPPG: 1,2-dipalmitoyl-sn-glycero-3-phospho- (1’-rac-glycerol) (sodium salt), DOTMA: 1,2-di-O-octadecenyl-3- trimethylammonium propane (chloride salt)
Table 1: Determination of encapsulation efficiency (%) for ceftazidime (3 mg/mL) in liposomes with various compositions; as hydrating solution phosphate buffer (pH 7.4) was used (n=3)
As ceftazidime has a polar character (log P = −1.6), deep immersion of ceftazidime molecules into the apolar bilayer is not suspected. Instead of this kind of interaction molecular forces between the lipid head groups and drug, e.g., through hydrogen bonds can be responsible for the encapsulation of ceftazidime. This presumption can be strengthened with the encapsulation efficiency data [Table 1]. For liposomes comprised of DPPC and DPPG, where the phospholipid bilayer is relatively rigid due to the completely saturated fatty acid, palmitic acid, the encapsulation efficiency was found to be the highest. The presence of cholesterol, acting as a fluidity increasing agent, did not lead to higher encapsulation of ceftazidime. It allows to suspect that membrane fluidity may not be the main factor influencing ceftazidime encapsulation.
While considering the hydrating solution, all the tested solutions resulted in almost similar encapsulation efficiencies [Table 2], with the highest mean value for ceftazidime liposomes prepared with phosphate buffer. However, the use of dextrose and sucrose for hydration may increase the possibility of microbial contamination of the liposomal preparations during storage.
| Hydrating solution | Encapsulation efficiency (%) of ceftazidime (±SD) |
|---|---|
| Phosphate buffer | 17.72±0.92 |
| 5% dextrose | 16.49±1.70 |
| 10% sucrose | 16.92±0.82 |
| 0.9% saline | 17.03±0.77 |
SD: Standard deviation, DPPC: 1,2-dipalmitoyl-sn-glycero-3-phosphocholine, DPPG: 1,2-dipalmitoyl-sn-glycero-3-phospho-(1’-rac-glycerol) (sodium salt)
Table 2: Determination of encapsulation efficiency (%) for ceftazidime in DPPC:DPPG (9:1 molar ratio) liposomes while varying the hydrating solution; pH=7.4 (n=3)
Taking into consideration one of the major needs of ophthalmic products – the formulation should possess physiologic pH value. The physiological tear pH range is 6.5-7.6; the mean value was 7.0. [5] Regarding the pH, the maximal ceftazidime stability in aqueous solutions occurs at pH 4.5-6.5. [4] On this basis the optimal pH for ceftazidime eye drops is about pH 6.5. Using osmotic phosphate buffers for hydration with pH 6.4; 7.4 and 8.4, significant difference cannot be observed between the ceftazidime encapsulation efficiency values (P > 0.05) [Table 3]. Thus, the criterion of optimal pH-value, being necessary for the formulation of ophthalmic preparations, can be fulfilled.
| pH of the buffer solution | Encapsulation efficiency (%) of ceftazidime (±SD) |
|---|---|
| 6.4 | 16.49±0.82 |
| 7.4 | 17.72±0.92 |
| 8.4 | 16.92±1.70 |
SD: Standard deviation, DPPC: 1,2-dipalmitoyl-sn-glycero-3- phosphocholine, DPPG: 1,2-dipalmitoyl-sn-glycero-3-phospho- (1’-rac-glycerol) (sodium salt)
Table 3: Determination of encapsulation efficiency (%) for ceftazidime in DPPC:DPPG (9:1 molar ratio) liposomes while varying the pH of hydrating phosphate buffer (n=3)
Comparing our ceftazidime encapsulation results with the literature data it is important to note, that ceftazidime and cefepime co-encapsulation into unilamellar vesicles was examined by Torres et al. [6] In their case, the average diameter of liposomes was 131.88 nm and encapsulation efficiency for cefepime and ceftazidime were 2.29% and 5.77%, respectively. [6] Our ceftazidime multilamellar vesicles (MLVs) with an average diameter of 2 μm prepared from DPPC show higher entrapment efficiency, 17.72 ± 0.92%, than small unilamellare vesicle (SUV) samples of Torres et al. This observation – beyond the question of co-encapsulation versus simple encapsulation – may be the consequence of the multilamellar structure applied in our present study. In our earlier experiments, the electron paramagnetic resonance signals out of the liposomes were quenched by paramagnetic relaxation and we observed for the incorporated aqueous volumes about 7% and 2% in case of MLVs and SUVs, respectively. [7-10] Ceftazidime encapsulation efficiency values in each case are higher than the ratio of the encapsulated aqueous volume highlighting the role of potential molecular interactions between carrier system and encapsulated drug and underlining the importance of further liposomal encapsulation studies.
References
- Kodym A, Hapka-Zmich D, Golab M, Gwizdala M. Stability of ceftazidime in 1% and 5% buffered eye drops determined with HPLC method. Acta Pol Pharm 2011;68:99-107.
- Dehghani AR, Fazel F, Akhlaghi MR, Ghanbari H, Ilanloo MR, Ahmadi-Azad D. Cefazolin-gentamicin versus vancomycin-ceftazidime eye drops for bacterial corneal ulcers: A J Ophthalmic Vis Res 2009;4:19-23.
- White NJ. Melioidosis. Lancet 2003;361:1715-22.
- Zhou M, Notari RE. Influence of pH, temperature, and buffers on the kinetics of ceftazidime degradation in aqueous solutions. J Pharm Sci 1995;84:534-8.
- Abelson MB, Udell IJ, Weston JH. Normal human tear pH by direct measurement. Arch Ophthalmol 1981;99:301.
- Torres IM, Bento EB, Almeida LC, Martins de Sá LZC, Lima EM. Preparation, characterization and in vitro antimicrobial activity of liposomal ceftazidime and cefepime against Pseudomonas aeruginosa strains. Braz J Microbiol 2012;43:3.
- Budai M, Szabó Z, Zimmer A, Szögyi M, Gróf P. Studies on molecular interactions between nalidixic acid and liposomes. Int J Pharm 2004;279:67-79.
- Kaszás N, Bozó T, Budai M, Gróf P. Ciprofloxacin encapsulation into giant unilamellar vesicles: Membrane binding and release. J Pharm Sci 2013;102:694-705.
- Budai L, Hajdú M, Budai M, Gróf P, Béni S, Noszál B, et al. Gels and liposomes in optimized ocular drug delivery: Studies on ciprofloxacin formulations. Int J Pharm 2007;343:34-40.
- Budai M, Chapela P, Budai L, Wales ME, Petrikovics I, Zimmer A, et al. Liposomal oxytetracycline and doxycycline: Studies on enhancement of encapsulation efficiency. Drug Discov Ther 2009;3:13-7.