Hypertensive Urgencies or Emergencies and Co-Morbidities in Bukavu Referral Hospitals: Clinical Profile, Management Regimens, Outcomes and Drug Related Problems
2 Department of Pharmacy, Faculty of Medicine and Pharmacy, Official University of Bukavu, DR, Congo
3 Department of Internal Medicine, University Clinics, Official University of Bukavu, DR, Congo
Citation: Mehta V, Desai N, Perwez A, Nemade D, Dawoodi S, Zaman SB. ACE Alzheimer’s: The Role of Vitamin A, C and E (ACE) in Oxidative Stress Induced Alzheimer’s Disease. J Basic Clin Pharma 2018;9:46-52.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Background: Hypertension is known as a silent disease ever complex to manage particularly in poor countries. Pharmacists may contribute to improving efficacy and safety. Objective: The study aimed at monitoring patients hospitalized for hypertensive urgencies or emergencies to evaluate the adequacy of treatment regimens and potential drug related problems. Methods: Retrospective/ prospective chart review of inpatients admitted for hypertensive crisis at two referral hospitals in Bukavu City, DR Congo. Primary outcomes were decrease in blood pressure, resistance to treatment and death. Results: The profile showed the prevalence of inpatients with hypertensive crisis was 9.7% (189/1948); that included 57% men and 43% women aged 23 to 88 years old whose 55% were on alcohol and tobacco. The majority (46%) had severe hypertension (BP>180/110) including 24.4% urgency cases and 76% emergency cases; the end-organ damages consisted of stroke (32%), heart failure (24.6%), chronic kidney disease (19.7%) associated or not with diabetes (39.8%); Co-morbid conditions were respiratory distress, urinary tract infection, sepsis, malaria, gastritis and cancer. Medication regimens included CCBs, ACEIs and ARBs in multidrug combination with diuretics, beta-blockers and a variety of products for co-existing health conditions. The treatment goal BP<140/90 was achieved in 87% while failure and death occurred in 10.6% and 2.4% respectively. Some drug related problems were encountered. Conclusions: The analysis found that the majority of patients are presenting with severe hypertension and in stroke condition showing that many people live with uncontrolled high blood pressure. The management outcome was satisfactory despite some medicines related problems encountered. There is a need to draft best standardized protocols to narrow the quality gap and avoid polypharmacy.
Keywords
Hypertension emergency; hypertensive urgency; management outcomes; drug related problems
Introduction
High blood pressure (HBP) termed hypertension (HT) consists of having systolic blood pressure (SBP)>140 mmHg and diastolic blood pressure (DBP)>90 mmHg. HT is a silent disease that discreetly claims uncalculated lives each year particularly after 50 years old. Some time ago, HT had been seen as a disease of affluence (DOA) in opposition to malaria or diarrhoea seen as diseases of poverty (DOP). However, current epidemiological studies show that HT strikes both rich and poor populations, leaving no race or social rank excluded.[1-5] About 15% of the adult population worldwide suffers from the disease which is directly or indirectly responsible for 10 to 20% of all annual deaths. [2] It accounts for 57 million disability adjusted life years (DALYS) or 3.7% of total DALYS.[2] Across the world, the prevalence of HT in WHO regions is highest in Africa, where it reaches 46% for both sexes combined, while the lowest prevalence is in Americas at 35%.[4,6,7]
Uncontrolled HBP may lead to severe hypertensive crisis consisting of hypertensive urgencies without end-organ damage (EOD) or hypertensive emergencies with EOD.[8,9] The incidence of conditions such as atherosclerosis, cerebral haemorrhagic stroke (CHS), left ventricular failure (LVF) or chronic kidney diseases (CKD) is correlated to the level of HBP.[2,8,9] The aetiology and complications of HBP have been associated to many risk factors such as obesity, heredity, tobacco and alcohol.[10,11] In spite of advances in the diagnosis and monitoring of patients, HT remains a complex disease ever difficult to manage particularly in tropical countries where it is often associated with other co-morbid illnesses like diabetes, malaria and infections.[6,7] According to guidelines of standards of care, the treatment of HT is aimed at normalizing BP in order to prevent complications.[12,13] The prevention by certain drugs and mortality criteria have been proven for BP thresholds of 160/95 mmHg levels or 140/80 mmHg in diabetics or after a stroke.[12,13] In all cases, a series of pharmacologic active anti-hypertensive molecules are used separately or in combination of which thiazide diuretics (TZDs), beta blockers (BBs), angiotensin converting enzyme inhibitors (ACEIs) or Angiotensin receptor blockers (ARBs), and calcium channel blockers (CCBs). These drugs are among highly dangerous or toxic xenobiotic that must be managed carefully to mitigate toxic hazards and gain optimal benefits. In specialized healthcare centres, standardized protocols of care are set up by therapeutic committees to better controlling clinical responses. In developing countries, the treatment is often less standardized and depends on the background or qualification of the personnel in charge of care.
In the Democratic Republic of the Congo (DRC), HT also is a very lethal disease and a serious public health concern.[14-17] According to the latest WHO data published in April 2011, hypertension deaths in DRC reached 5,807 or 0.65% of total deaths. It is the most indisputable cardiovascular risk factor. The age adjusted Death Rate of 27.72 per 100,000 of population ranks DRC #85 in the world.[16] The prevalence in Southern Kivu province was estimated at 30-40%.[15] Here, hypertensive patients are mostly managed by general practitioners. Little is known about HE/HU profile and management. This study has been undertaken to assess the profile of patients with HU/HE episodes, analyse how well they are pharmacologically managed in respect of common standards of care and highlight the “quality gap†defined as the difference between present treatment success rates and those thought to be achievable using hypertension best practices described by international societies of hypertension like European Society of Hypertension (ESH) and US National joint committee (NJC).[18,19]
Methods
Study design and patients
The study consisted on one part of a retrospective analysis of data extracted from patients hospitalized in 2015 in internal medicine services at two referral hospitals in Bukavu city namely ‘Hospital provincial de reference de Bukavu’ (HPGRB) and ‘Hopital general de reference de Panzi’ (HGRP). On another part, it consisted of a prospective monitoring of inpatients routinely treated for HE/HU in the two hospitals during the year 2016. Patients were treated as usual without interference of the investigators pharmacists. Data were collected exclusively from patients’ medical notes. Pregnant women and patients discharged in 24 hours were excluded for analysis considering that they were not at high risk.
Variables
Age, sex, risk factors, BP levels, comorbidities, symptoms, medications and complaints were collected. HT grade was classified as Stage 0 (SBP=120-139, DBP=80-89 mmHg); Stage 1 (SBP=140-159, DBP=90- 99); Stage 2 (SBP=160-179, DBP=100-110); Stage 3 (SBP>180, DBP>110). Therapeutic efficacy meant BP goal< 140/90. Drug related problems meant whether patients got a wrong drug for their conditions, received more or less than the dose required, got wrong or no drug taken, experienced adverse drug reaction, or there were manifest or potential drug-drug interactions.
Statistical data analysis
The collected data was analysed with Microsoft Excel Windows and SPSS software v20 for descriptive statistics. Statistical significance of differences between groups, where applicable, was set at p< 0.05 using Pearson Fisher’s Test.
Results
Clinical profile of patients
The annual hospital prevalence of HE/HU was 9.7% (189/1948). Table 1 presents patients’ demographics and clinical features. Out of 123 valid cases analysed, there were 71(57.7%) men vs. 52(42.3%) women. The majority 59(48%) were 60-88 years old. About 55.5% were alcohol and/or tobacco users. At the admission, 57.7% presented with BP values higher than 180/110 mmHg (stage-III). For clinical features, 24.4% consisted of HU against 75.6% HE. The signs of EOD were stroke (31.7%), nephropathies (19.5%) and heart diseases (24.4%). For HT symptoms, 77.2% presented headache, followed by dizziness (55.3%), fatigue (52.8%), palpitation (48%), blurred vision (30.9%), dyspnoea (17.1%), and coma (8.9%). During the treatment, patients complained of vomiting (8.1%), cough (7.3), fever, lumbar pain, chest pain, diarrhoea or constipation, dehydration, dyspepsia, etc. Those could be either symptoms of co-morbid conditions or drug related side effects. Comorbidities included diabetes (39.9%), urinary infection (15.4%), all-type pulmonary problems (13.8%), malaria (4.9%), sepsis (5.7%), cancer (5.6%), and gastritis (6.5%) among others.
| Variables | % | Variables | % | Variables | % |
|---|---|---|---|---|---|
| Hospitals | Gender | Age –years | |||
| HPGRB | 45.5 | Female | 42.3 | 23-39 | 15.4 |
| HGRP | 54.5 | Male | 57.7 | 40-59 | 36.6 |
| 60-99 | 48.0 | ||||
| Risk factors | Disease stage | End-organ damage | |||
| No | 45.5 | 0 SBP 120-139 | 4.1 | No | 24.4 |
| Alcohol | 39.0 | 1 SBP 140-159 | 13.0 | Stroke | 31.7 |
| Tobacco | 4.1 | 2 SBP 160-179 | 25.2 | Heart Failure | 24.4 |
| Both | 11.4 | 3 SBP 180-200 | 57.7 | Kidney Disease | 19.5 |
| Symptoms | Complaints | Co-morbidities | |||
| Headache | 77.2 | Vomiting | 8.1 | No | 56.9 |
| Dizziness | 55.3 | Cough | 7.3 | Diabetes | 39.9 |
| Fatigue | 52.8 | Fever | 5.7 | Urinary Infection | 15.4 |
| Palpitation | 48.0 | Chest pain | 5.7 | Malaria | 4.9 |
| Blurred Vision | 30.9 | Epigastric pain | 5.7 | Gastritis | 6.5 |
| Dyspnoea | 17.1 | Diarrhoea | 4.1 | Sepsis | 5.7 |
| Coma | 8.9 | Lumbar pain | 4.1 | Asthma | 4.0 |
| Lung-oedema | 4.1 | Constipation | 2.4 | Pneumonia | 2.4 |
| Hemiplegic | 3.3 | Dysuria | 3.3 | Benin Prostate H. | 2.4 |
| Dysarthria | 3.3 | GI Haemorrhage | 2.4 | Pyelonephritis | 1.6 |
| Ear rings | 3.3 | Hematuria | 1.6 | Rabdomyosarcoma | 1.6 |
| Pleurisy | 2.4 | Dyspepsia | 1.6 | Adenocarcinoma | 0.8 |
| Epistaxis | 2.4 | Dehydration | 1.6 | Hepatocarcinoma | 0.8 |
| Cardiac asthma | 1.6 | Polyarthralgia | 0.8 | - | |
| Leg oedema | 1.6 | Migraine | 0.8 | - |
Table 1: Repartition of hypertensive patients by clinical profile in Bukavu referral hospitals
Management therapeutic regimens
Table 2 presents examples of antihypertensive regimens in monotherapy or combination of two to five molecules. In total, CCBs were the most used ((97%) leaded by amlodipine, followed by ACEIs (52%) and ARBs (3%), diuretics (36%) and beta-blockers (8%). The CCBs included amlodipine(Aml), nicardipine(Nic), and nifédipine(Nif). ACEIs and ARBS consisted of enalapril (Ena), captopril(Cap), and losartan(Los). BBs included atenolol(Ate) and bismolol(Bis), The diuretics used were furosemide(Fur), hydrochlorthiazide(hyd) and spironolactone or Aldactone(Ald).
| Medicines | N | Medicines | N | Medicines | N | Medicines | N |
|---|---|---|---|---|---|---|---|
| Monotherapy | Bitherapy | Bitherapy | Polytherapy | ||||
| Aml10 | 25 | Aml10Cap50 | 7 | Aml10Fur180 | 2 | Aml5Cap75Ate50 | 1 |
| Aml5 | 24 | Aml10Cap75 | 5 | Cap50Fur20 | 2 | Nif40Fur80Ena5 | 2 |
| Cap50 | 9 | Aml5Cap75 | 1 | Ena10Fur40 | 2 | Aml10Ena5Bis2.5 | 2 |
| Cap75 | 6 | Aml10Cap25 | 3 | Ena2.5Fur60 | 1 | Cap75Fur80Ate50 | 1 |
| Cap25 | 3 | Nic10Cap150 | 2 | Ena5Fur20 | 1 | Aml10Ate100Fur120 | 1 |
| Cap100 | 1 | Aml10Ena10 | 3 | Nic10Fur40 | 2 | Aml10Fur60Ena5 | 1 |
| Ena10 | 7 | Aml10Ena5 | 7 | Ena5Fur60 | 1 | Aml10Ena5Bru20 | 1 |
| Ena5 | 4 | Aml5Ena20 | 2 | Nif40Fur120 | 1 | Aml10Fur40Ena5 | 1 |
| Nic10 | 17 | Nif40Ena10 | 2 | Bis10Fur80 | 1 | Aml10Fur40Los100 | 1 |
| Nif40 | 10 | Nic10Cap75 | 2 | Aml10Fur60 | 1 | Nif40Fur60Ena5 | 1 |
| Nif20 | 1 | Nif20Ena5 | 1 | Aml5Fur360 | 1 | Ena5Fur40Ald25 | 1 |
| Bis5 | 3 | Aml5Cap50 | 2 | Aml10Fur40 | 3 | Nic10Nif40Bis10 | 2 |
| Bis10 | 3 | Aml10Nic10 | 1 | Cap50Fur60 | 3 | Nif20Ena5Car12.5 | 1 |
| Fur20 | 3 | Nic4Bis5 | 2 | Aml5Fur80 | 2 | Nif20Fur80Ena5 | 1 |
| Fur40 | 1 | Nic10Ate50 | 2 | Nif40Fur80 | 3 | Nif40Fur40Bis10 | 1 |
| Nif40Fur40 | 4 | Aml10Fur80Bis5 | 1 | ||||
| Ena2.5Hyd12.5 | 2 | Aml10Mox0.2Irb150 | 1 | ||||
| Aml10Hyd25 | 1 | Nic5Nif40Bis10 Nic4Bis5 | 1 | ||||
| Aml10Fur120 | 4 | Nif40Fur60Ena5Ald25Cap50 | 1 | ||||
| Aml10Cap75Ena10Ate100Fur80 | 1 |
Table 2: Regimens of antihypertensive medicines prescribed (n=123)
As shown in the table, various doses were used depending on the patients. For instance 25 patients received amlodipine 10 mg (Aml10); 24 patients received Am5; 9 patients received Cap50. In biotherapy, CCBs were combined with ACEIs (Aml10Ena5) or with diuretics (Cap50Fur20), or with BBs (Nic10Bis5). Examples of associating more than two are (Aml10 Cap75 Ena10 Ate100 Fur80).
The antihypertensive medicines were often given in association with antihyperlipidemiants (Atorvastatin), heparinates (Exanoparine), hemostatics (tranexamic acid), antiplatelets (Clopidogrel), and other cardiovascular agents like atropine, adrenalin, nitroglycerin (Table 3). Besides antihypertensive and other cardiovascular medicines described, co-morbidities were managed with a variety of specific pharmacological products in polypharmacy, mainly consisting of antidiabetics (Insulin actrapid or NPH), painkillers (Paracetamol, Tramazol), antimicrobials (Ceftriaxone, ciprofloxacin), antiulcer (omeprazol), respiratory medications (salbutamol), vitamins (C and E), and anticancer (Tamoxifen). Individual doses fell within the recommended ranges
| Medicines | % | Medicines | % | Medicines | % |
|---|---|---|---|---|---|
| Hemostasis | Heart | Diabetes | |||
| AAS junior | 20.3 | Adrenalin | 1.6 | Insulin(A/NPH) | 16.3 |
| Clopidogrel (Plavix) | 2.4 | Atropine | 0.8 | Metformin | 6.5 |
| Simvastatin | 3.3 | Nitrolingual | 1.6 | Glibenclamide | 3.3 |
| Atorvastatin (Lolip) | 4.9 | Trinitrine patch | 0.8 | ||
| Dicynone | 3.2 | Cedocard | 1.6 | ||
| Enoxaparine, Fraxiparine | 4.2 | Mannitol | 4.9 | ||
| Tranexamic acid (Exacyl) | 1.6 | ||||
| Antibiotics | Gastrointestinal | Pain & Bronchitis | |||
| Ciprofloxacin | 24.4 | Rabeprazole | 22 | Paracetamol | 27.6 |
| Ceftriaxone | 21.1 | Omeprazole | 5.7 | Tramadol | 5.7 |
| Amoxicillin | 7.3 | Polygel Sp | 3.3 | Ibuprofen | 0.8 |
| CoArtem® | 4.9 | Metoclopramide | 5.7 | Diclofenac | 0.8 |
| Augmentin® | 3.9 | Mebeverine | 3.3 | Salbutamol | 3.3 |
| AzIthromycin | 4.9 | Actapulgite | 1.6 | Dexamethasone | 2.4 |
| Furadantin | 4.1 | Buscopan | 1.6 | Promethazine | 2.4 |
| Metronidazole | 4.1 | Lactulose | 1.6 | Diphenidramine | 1.6 |
| Cefotaxime | 2.4 | Gaviscon | 1.6 | Prednisolone | 1.6 |
| Clarithromycin | 1.6 | Maalox | 1.6 | Budesonide Spray | 0.8 |
| Erythromycin | 1.6 | Ranitidine | 1.6 | Carbocystein syrop | 0.8 |
| Fluconazole | 1.6 | Sucralfate | 1.6 | Syrop mucolytic | 0.8 |
| Rovamycin | 1.6 | Bisacodyl | 0.8 | Salbutamol Spray | 0.8 |
| Cloxacillin | 0.8 | Cimetidine | 4.1 | Beclomethasone Spray | 1.8 |
| Gentamicin | 2.4 | Meronia | 0.8 | Desloratadine | 0.8 |
| Mebendazole | 0.8 | Microlax | 0.8 | Cortancyl (prednisone) | 0.8 |
| Amitriptyline | 0.8 | Domperidone | 2.4 | ||
| Central nervous | Vitamins | Cancer | |||
| Clomipramine | 1.6 | Vitamin C | 27.6 | Tamoxifen | 0.8 |
| Diazepam | 0.8 | Vitamin E | 10.6 | ||
| Gamalate B6 | 0.8 | Kayexalate-Ca | 2.4 | ||
| Bromazepam | 0.8 | Magne B6 | 2.4 | ||
| Phenobarbital | 0.8 | Fefol | 0.8 | ||
| Piracetam | 1.6 | Gluconate-Ca | 4.8 | ||
| Nucleo CMP | 0.8 | Tribex fort® | 4.1 |
Table 3: Percentage (n=123) of medicines prescribed for HT co-morbidities
Management outcomes
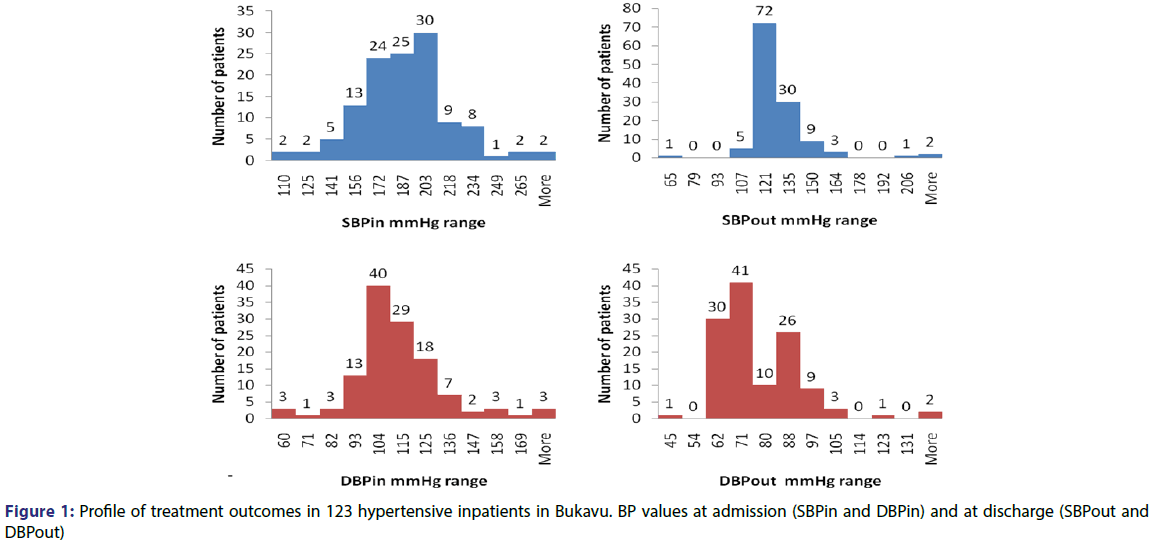
Figure 1 summarizes BP values at admission (SBPin-DBPin) and at discharge (SBPout-DBPout) time. The treatment success was appreciated by the profile of BP at discharge compared to admission day. The mean ± SD of SBPin was 181.67 ± 29.43 (110-280) compared to SBPout of 123.47 ± 18.76 (65-220). The mean ± SD of DBPin was 107.90 ± 20.24 (60-180) compared to DBPout of 73.54 ± 14.03(45-140). The difference was statistically significant (p=0.001).
Profile of treatment outcomes in 123 hypertensive inpatients in Bukavu
BP values at admission (SBPin and DBPin) and at discharge (SBPout and DBPout).
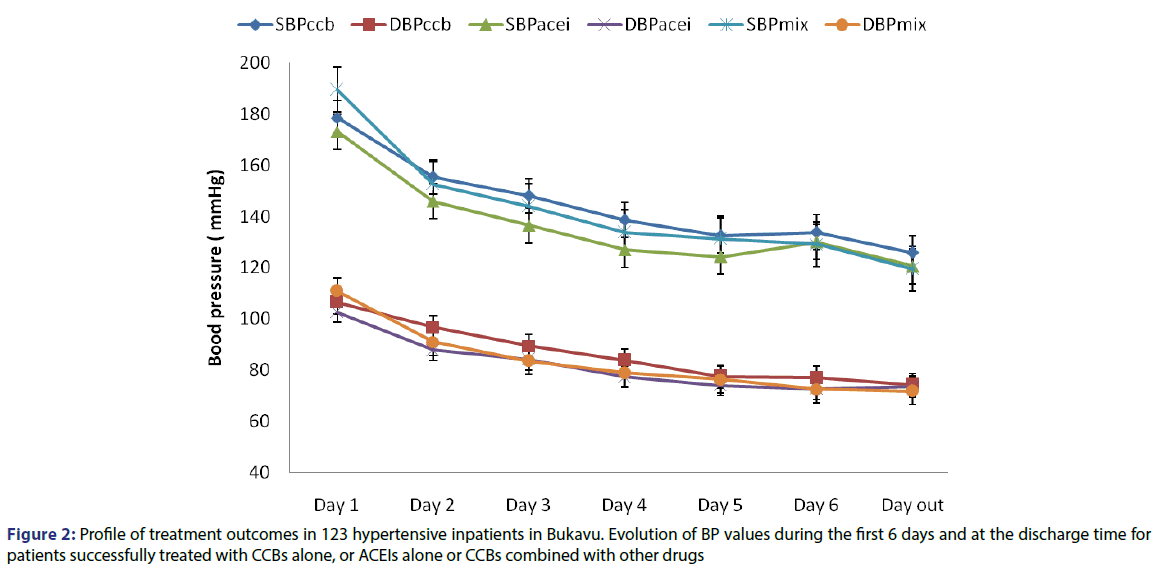
Effect of regimens on outcomes
Figure 2 presents the curves describing the evolution of treatment during the 6 first days and at the discharge time which varied from day 5 to day 30. We compared CCBs based to ACEIs based regimens. SBP and DBP for CCBs (SBPccb and DBPccb) were compared to SBP and DBP for ACEIs (SBPacei and DBPacei) and to SBP and DBP of multiple associations (SBPmix and DBPmix).
There were no significant differences for patients treated with CCBs and ACEIs even though the decrease was slightly rapid under ACEIs.
Discussion
The proportion of hypertensive inpatients approached 9.7% in the internal medicine services of the two hospitals. The HT prevalence in the entire population of Southern Kivu province has been estimated to 41.4% in urban vs 38.1% in rural areas.[15] The finding in Bukavu shows that many people are living with HT as silent condition and remained ignorant about their status and untreated; they lately rush to hospital in hypertension urgency or emergency episodes. In fact, the majority of patients present with hypertension stage III(BP>180/110) including 24% HU and 76% HE. In a study by Zampaglione et al.[9] Done in emergency room, HU accounted for 76% and HE for 24%, the reverse of our finding. In our hubs the majority of patients present with end-organ damages consisting of haemorrhagic or ischemic stroke (32%), heart failure (14.6%), chronic kidney disease (9.7%), and hypertensive encephalopathy (4.9%). This is consistent with other studies showing that the most common clinical presentations of HE are cerebral infarction (24.5%) associated with intracranial haemorrhage, aortic dissection, congestive heart failure and acute myocardial infarction (12%), pulmonary oedema (22.5%) and hypertensive encephalopathy (16.3%).[20-28] Disease symptoms included dizziness, fatigue, headache, nosebleed, tachycardia, heart palpitations, blurred vision and ear ringing while the main co-morbidities were diabetes (38.8%), respiratory distress, urinary tract infection, sepsis, malaria, gastritis and cancer.
The study sample comprised of 57.7% of men against 42.3% women, supporting world statistics that show both sexes would be exposed in the same way, whatever the general trends show that men are somehow more exposed than women.[1,4] The population above 60-88 years old was the most affected by HBP in this study (48%), consistent with many studies showing that HT strikes less than 2% of patients under 20 years and more than 40% of patients over 50 years old.[1] About 50% of patients were alcohol drinkers and tobacco smokers. Alcohol or smoking can increase the risk of complications when associated with aging.
The JNC8 recommends reduction of BP levels below 150/90 mm in patients aged 60 years or older, reduction below 140/90 mm Hg in patients younger than 60 years as well as those older than 18 years with either chronic kidney disease (CKD) or diabetes.[19] With the regimens delivered in Bukavu hospitals, the therapeutic goal BP< 140/90 was achieved in 87% of patients within 6 to 30 days after the treatment was initiated. Failure and death affected 12.6% and 2.4% respectively within the 30 days of follow-up. Resistant hypertension also is a common clinical problem faced by both primary care clinicians and specialists. While the exact prevalence of resistant hypertension is unknown, clinical trials suggest that it is not rare, involving perhaps 20% to 30% of study participants.[2]
The treatment success rate is not too widely different with regard to other studies.[29-31] However, some gap was observed with regard to contemporary recommendations[32-35] applicable to HE/HU management. To manage HEs, labetalol an alpha-beta-blocking agent has proven to be quite beneficial in the treatment of patients as well as fenoldopam, a peripheral dopamine-1-receptor agonist given as initial IV dose of 0.1 µg/kg/min titrated every 15 min. No patient was given labetalol or fenoldopam in this study. In hypertensive encephalopathy, the preferred medications are labetalol, nicardipine, esmolol. Only nicardipine was used alongside other CCBs and ACEIs. Direct vasodilators like nitroprusside and hydralazine are contra-indicated in this case. In general, direct vasodilators were not used in any case.
In acute heart failure, the preferred medications are IV nitroglycerin or sublingual nitroglycerin and IV enalaprilat.[32] Here, Nitrolingual was prescribed in patients with heart failure and pulmonary oedema. One NJC8 recommendation stipulates that regardless of race or diabetes status, in patients 18 years or older with CKD, initial or addon therapy should consist of an ACE inhibitor or ARB and do not use an ACE inhibitor in conjunction with an ARB in the same patient. In our cases, patients presenting CKF were initiated only on amlodipine or nicardipine. Certain beta blockers and thiazides in combination increase insulin resistance (risk of diabetes) with increased triglycerides and congestive heart failure.[30-32] Here, only hydrochlorthiazide was used as thiazide but not in combination with BBs. Furosemide (Lasix) which is loop diuretic was preferred to thiazide-type. This is because in the country, the only best known diuretic is Lasix. In hypertension and Angor, CCBs with tachychardisant effect as Amlor LP should be avoided. However Amlor was unfortunately the agent of choice in many patients despite the co-existing cardiac illnesses. In the majority of our patients, the treatment was initiated with amlodipine, nicardipine or enalapril. Alpha-receptor inhibitors are most often prescribed in case of failure of at least two other treatments; centrally acting alpha-2 agonists and direct vasodilators have place in special and emergency episodes. No alpha-1 blockers were indicated in resistant patients and only 1 patient was treated with Moxonidine a central acting congener to clonidine.
Many studies have showed that drug-related problems are prevalent and cause considerable patient morbidity and in some cases death, as well as increased health care expenditures. The common classification of DRPs has a hierarchical structure with six main categories (drug choice, dosing, adverse drug reaction, interaction, drug use and other) and 12 subcategories.[36,37] For this study, we adopted the structure comprising 8 DRPs and the following observations can be made. DRP1. Inappropriate Medication; the patient takes or receives a drug other than the one required. The result showed that the medications prescribed were drugs of choice in the treatment of all-types hypertension and comorbidities. Diabetes was managed with insulin, glibenclamide and metformin. For malaria, only Artemether/ Lumefantrine (CoArtem) was prescribed. Ciprofloxacin and ceftriaxone were the major antibiotics. Proton pump inhibitors like omeprazole, antihistamine-H2 like ranitidine, or antacids like Maalox were used for ulcer management. Some bronchodilators and anticonvulsants were also prescribed alongside painkillers and anti-anaemia drugs in case. Although all medicines used sounded appropriate, it has been however difficult to agree whether all those were needed.
DRP2: the patient needs a drug, but does not receive it. In the majority of cases, patients received their first choice treatment, but in all cases. The following example illustrates the gap. Mr AD, aged 54 years old, presented at the hospital with Grade III hypertension and complicated stroke with intracranial effusion, headache and severe pain. At the entrance BP was 275/178 mmHg; Rx initiated with Nicardipine inj 1x10 mg, 1x1000 mg paracetamol inj, tramadol inj 1x100 mg. At day 2, BP dropped to 160/97 mmHg under same treatment; at day 3, the patient died with BP 220/120 mmHg. Whatever the case was severe, it sounds no emergency protocol was applied.
DRP3 and DRP4: The patient takes or receives the correct drug, but at too low or too high doses. The standard doses used were in the recommended ranges. However there was no sign of individual adjustment on the basis of kidney failure. Ms X Age 63 years presented with HTA grade III complicated with Ischemic Stroke. At the entrance the patient had a speech problem, impotence of inferior members, with a BP 220/150. At the entrance she received Nicardipine 1x10 mg inj; at day 2: BP was 220/130 mmHg and received again Nicardipine 1x10 mg inj; at day 3 BP dropped to 180/120 mmHg, and received Captopril 3x25 mg, Atenolol 1x50 mg and Amlodipine 1x5 mg; at day 4, BP was 170/120 mmHg and received Lasix 2x40 mg, Captopril 3x25 mg, Atenolol 1x50 mg; at day 5, BP was 180/120 mmHg and received same treatment as day 4; at day 6, BP was 200/120 mmHg and received Captopril 3x25 mg, Nicardipine inj 1x10 mg; at day 7, BP was 180/120 mmHg and received Lasix 2x40 mg, Enalapril 2x5 mg, Atenolol 2x50 mg, Amlodipine 1x10 mg, Captopril 3x25 mg; at day 8 the patient died in a collapse with BP 65/45 mmHg. This case illustrates wrong use of associations and dosing.
DRP5. The patient does not take or does not receive the medication as prescribed. Our sample consisted of inpatients in Internal Medicine Service. Therefore, we assumed that the compliance or adherence was excellent because the administration was done by nurses. However, this has not been confirmed since all patients were required to pay cash medicines mostly outside the hospital. The situation is almost similar in many poor countries. Also after exit to home, it is difficult to make a valuable judgment on adherence as the treatment is costly and demanding. Many medicines were prescribed in trade name® that are expensive, like Efferalgan (paracetamol); Dafalgan (paracetamol); Largactil (chlorpromazine); Lexotan (bromazepam); Nootropil (piracetam); Cortancyl (prednisone), Diabetaz (glibenclamide), Vermox (mebendazole), Glucophage (metformin), Gliben (glibenclamide), Ipprosec (rabeprazole), Duphalac (lactulose), Ulcar (sucralfate), Spasfon (mebeverine), Clamoxil(amoxicillin), Nolvadex (tamoxifen), Fefol (iron and folate).
RP6: Adverse reaction. A number of complaints were noticed like cough, diarrhoea, constipation, vomiting, epigastralgia, etc. It was difficult to establish a decisive link between those complaints and the medications received. Nevertheless, coughing is characteristic of ACEI agents; headache and palpitations are associated with CCBs.[38,39]
DRP7: Interactions. The patient undergoes an interaction between the drug and another drug, food, or a biological test. Some possible interactions could occur even though not evidenced in this case. Combination of statins (simvastatin, atorvastatin) and inhibitors of CyP450 3A4 can lead to serious liver and muscle side effects. Aldactone interacts with ACE inhibitors and ARBs (addition of hyperkalemia effect with doses of 12.5 to 50 mg per day). Their antihypertensive effects may be increased in combination with antipsychotics, tricyclic antidepressants.[40-42]
DRP8: Unnecessary medications. Several cases have been met where the combination of vitamin C and vitamin E or redundancies were systematically given without justification.
Conclusion
The study revealed high level of hypertensive emergency, high frequency of all-type stroke, diabetes and infections. The medicines used and outcomes were satisfactory despite some drug related problems. However, there is a need to fix best standardized protocols susceptible to further narrow the quality gap. Educational campaign about early blood pressure checking over 50 years is of great importance to reduce the high frequency of stroke observed.
Ethics approval and consent to participate
The protocol of the study was approved by the Research Ethical Committee of the Faculty of Medicine and Pharmacy of the Official University of Bukavu. The consent to participate was Not Applicable.
Consent to publish
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interest
The authors declare that they have no competing interests.
Funding
No external funds.
Author Contribution
JNK, BB, and JDS designed research; BB and JDS conducted research; JNK, BB, JDS and DM analyzed data; JNK and JDS wrote the paper and had primary responsibility for final content. All authors read and approved the final manuscript.
Acknowledgement
The authors wish to thank the research nurses, medical coordinators and operations staff as well as patients included in this study.
REFERENCES
- Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Somnath Chatterji S. Hypertension among older adults in low and middle-income countries: prevalence, awareness and control. Int J Epidemiolo 2014;43:116-28.
- WHO 2016. Available from: http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/
- World Health Organization. Global status report on non-communicable diseases 2017 Available at: http://apps.who.int/iris/bitstream/10665/128038/1/9789241507509_eng.pdf?ua=1
- Kazem R, Connor AE, Stephen M. The Epidemiology of Blood Pressure and Its Worldwide Management. Circulation Res 2015;116:925-36.
- WHO 2016 http://ish-world.com/downloads/pdf/global_brief_hypertension.pdf
- Lemogoum D, Seedat YK, Mabadeje AF, Mendis S, Bovet P, Onwubere B, et al. Recommendations for prevention, diagnosis and management of hypertension and cardiovascular risk factors in sub-Saharan Africa. J Hypertens 2000;21:1993.
- Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovascular Disorders 2013;13:54.
- Martin JF, Higashiama E, Garcia E. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol 2004;83:131.
- Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension 1996;27:144.
- Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G. Alcohol consumption and the incidence of hypertension: The Atherosclerosis Risk in Communities Study. Hypertension 2001; 37:1242-50.
- Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 2001; 38:1112-7.
- James PA, Oparil S, Carter BL. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20.
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281-357.
- M’Buyamba KJR, Biswika T, Thijs L, Tshimanga GM, Ngalula FM, Disashi T, et al. In-hospital mortality among Black patients admitted for hypertension-related disorders in Mbuji Mayi, Congo. Am J Hypertens 2009;22:643-8.
- Katchunga BP, Mbuyamba KJR, Masumbuka EB, Lemogoum D, Kashongwe MZ, Degaute JP, et al. Hypertension in adult Congolese population in Southern Kivu: Results of the Vitaraa Study. La Presse Médicale 2011;40.
- Longo-Mbenza B, Ngoma DV, Nahimana D. Screen detection and the WHO stepwise approach to the prevalence and risk factors of arterial hypertension in Kinshasa. Eur J Cardiovasc Prev Rehabil 2008;15:503-8.
- Lulebo AM, Mapatano MA, Kayembe PK, Mafuta EM, Mutombo PB, Coppieters Y, et al. Assessment of hypertension management in primary health care settings in Kinshasa, Democratic Republic of Congo. BMC Health Services Res 2015;15:573.
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the Eur Society of Cardiolo. J Hypertens 2007;25:s1105–87.
- JNC8. Evidence-Based Guideline for the Management of High Blood Pressure in Adults 2016. http://jamanetwork.com/journals/jama/fullarticle/1791497 .Access Nov 12
- Johnson W, Nguyen ML, Patel R. Hypertension crisis in the emergency department. Cardiol Clin 2012;30:533.
- Börgel J, Springer S, Ghafoor J. Unrecognized secondary causes of hypertension in patients with hypertensive urgency/emergency: prevalence and co-prevalence. Clin Res Cardiol 2010;99:499.
- Elliott WJ. Clinical features in the management of selected hypertensive emergencies. Prog Cardiovasc Dis 2006;48:316.
- Anderson CS, Heeley E, Huang Y. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med 2013;368:2355.
- Hemphill JC 3rd, Greenberg SM, Anderson CS. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/Ame Stroke Assoc. Stroke 2015;46:2032.
- Elliott WJ, Weber RR, Nelson KS. Renal and hemodynamic effects of intravenous fenoldopam versus nitroprusside in severe hypertension. Circulation 1990;81:970.
- Davila EP, Hlaing WM. Comorbidities of Patients with Hypertension Admitted to Emergency Departments in Florida Hospitals Florida Public Health Review 2008;5:84-92.
- Kolo PM, Jibrin YB, Sanya EO, Alkali M, Kio IBP, Moronkola RK, et al. Hypertension-related admissions and outcome in a tertiary hospital in Northeast Nigeria. Int J Hypertens 2012.
- AHRQ. Closing the Quality Gap: A Critical Analysis of Hypertension Care Strategies Advancing Excellence in Health Care 2017. https://www.ahrq.gov/research/findings/evidence-based-reports/hypergap3tp.html
- Hirschl MM, Seidler D, Müllner M, Kürkciyan I, Herkner H, Bur A, et al. Efficacy of different antihypertensive drugs in the emergency department. J Hum Hypertens 1996;10:3:S143-6.
- Salkic S, Selmira B, Mujanovic OB, Ljuca F, Karabasic A, Mustafic S, et al. Emergency Room Treatment of Hypertensive Crises. Med Arch 2015;69:302-6.
- Brody A, Rahman T, Reed B, Millis S, Ference B, Flack JM, et al. Safety and Efficacy of Antihypertensive Prescription at Emergency Department Discharge. Academic Emergency Med 2015;22:632-5.
- Hopkin C. Hypertensive Emergencies 2017. http://emedicine.medscape.com/article/1952052-overview
- Chen JMH, Heran BS, Perez MI, Wright JM. Blood pressure lowering efficacy of beta-blockers as second-line therapy for primary hypertension. Cochrane Database Syst Rev 2010;20.
- Arguedas JA, Leiva V, Wright JM. Blood pressure targets for hypertension in people with diabetes mellitus. Cochrane Database Syst Rev 2013;30:CD008277.
- Ninomiya T. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ 2013; 3:347:f5680.
- Blix HS, Viktil KK, Reikvam A. The majority of hospitalized patients have drug-related problems: results from a prospective study in general hospitals. Eur J Clin Pharmacol 2004;60: 651-?8.
- Mannheimer B, Ulfvarson J, Eklof S. Drug-related problems and pharmacotherapeutic advisory intervention at a medicine clinic. Eur J Clin Pharmacol 2008;62:1075-81.
- Mannesse CK, Derkx FH, de Ridder MA. Contribution of adverse drug reactions to hospital admission of older patients. Age Ageing 2000;29:35-9.
- Yacob GT. Drug Side Effect Symptoms and Adherence to Antihypertensive Medication. Am J Hypertens 2015;29:772-9.
- Adeyemo A, Tayo BO, Luke A, Ogedegbe O, Durazo-Arvizu R, Cooper RS, et al. The Nigerian-Antihypertensive Adherence Trial (NA-HAT): a community based randomized trial. J Hypertens 2013;31:201-7.
- Yi Chun W, Tsung Cheng H, Chu Lin C, Jung Lun W, Te Chao F. Risks of Adverse Events Following Coprescription of Statins and Calcium Channel Blockers. A Nationwide Population-Based-Study. Medicine (Baltimore) 2016;95:e2487.
- Van Zwieten PA. Interactions between antihypertensive agents and other drugs 2017. http://www.eshonline.org/esh-content/uploads/2014/12/17_Newsletter-Interactions-Between-Antihypertensive-Agents-and-Other-Drugs.pdf