Evaluation of antidiabetic prescriptions, cost and adherence to treatment guidelines: A prospective, cross-sectional study at a tertiary care teaching hospital..
- *Corresponding Author:
- Dr. Kartik N. Shah
Department of Pharmacology, Smt. NHL Municipal Medical College, Ellisbridge, Ahmedabad - 380 006, Gujarat, India.
E-mail: knshah10@gmail.com
Abstract
Introduction: Diabetes mellitus is on alarming rise in India. Drug utilization studies help to identify the adherence to standard treatment guidelines and to evaluate the rational drug usage. Objective: To study prescription pattern, calculate the cost of antidiabetic drugs and to evaluate the adherence to treatment guidelines in diabetic patients attending the medicine outpatient department in a tertiary care teaching hospital. Materials and Methods: A prospective observational study was carried out for a period of 5 months. The diabetic patients who visited the medicine outdoor department were included. Demographic data and complete prescription details were recorded in the structured case record form. Cost of the drug therapy was calculated from the patient’s bills. Indian Council for Medical research guidelines-2005 for diabetes management was used to evaluate the adherence. Results: A total of 250 patients were enrolled in the study with mean age 57.91 ± 9.37. Out of 250 patients 126 (50.4%) were male and rest were female. A total of 1,391 drugs were prescribed, with mean of 5.56 ± 2.52 drugs and out of which 539 drugs were antidiabetics with mean of 2.18 ± 0.96. In monotherapy, metformin was frequently 218 (40.45%) prescribed. Glimepiride and metformin was the most frequently prescribed in 119 (76.28%) out of 156 antidiabetic drug combinations. Most commonly used drugs other than antidiabetics were aspirin 146 (18.9%) and atorvastatin 119 (15.41%). Mean cost of therapy for a month for a diabetic patient was 354.60 ± 305.72 INR. Majority 209 (83.6%) of prescriptions was in accordance to guidelines. Conclusion: Metformin was the most frequently prescribed drug in the diabetes patient. Metformin and glimeperide being the most frequent combination used. Majority of the prescriptions followed standard guidelines.
Keywords
Adherence, antidiabetic drugs, diabetic outpatients, drug utilization
Introduction
Six percent of the world population is affected by diabetes mellitus (DM) which is a chronic metabolic disorder. [1] The WHO defines diabetes mellitus as “A metabolic disorder of multiple aetiology characterized by chronic hyperglycemia with disturbances of carbohydrate, fat and protein metabolism resulting from defects in the insulin secretion, insulin action, or both”. [2] A survey on Indian population shows that 4% of the adults suffered from diabetes mellitus in the year 2000 and it is expected to rise to 6% by the year 2025. [3] In developing country like India, the majority of diabetics are in the age group of 45-64 years in contrast to developed countries it is highly prevalent in more than 65 years of age. [4] The management of type 1 diabetes mellitus depends mainly on insulin, whereas the oral antidiabetic drugs (OADs) are the first line treatment for type 2 diabetes mellitus. [5] Complications due to hyperglycemia in diabetes mellitus can be prevented by using rational use of oral antidiabetic drugs (OADs) and insulin. [6] Rational use of the drugs is a complex issue with a goal that is difficult to achieve, defined as follows: “That patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements for an adequate period of time, and at the lowest cost to them and their community”. [7]
Rational use of the drugs in populations can be effectively studied with drug utilization reviews. The World Health Organization (WHO) defines “drug utilization” as the marketing, distribution, prescription and use of the drugs in a society considering its consequences, either medical, social, and economic. Drug utilization studies is an invaluable investigational resource to study pharmacoepidemiology, pharmacovigilance, pharmacoeconomics and pharmacogenetics. [8] The World Health Organization (WHO) has formulated a set of “core prescribing indicators” for improvement in the rational drug use in the outpatient practice. It includes the prescribing indicators, the patient care indicators and the facility indicators. [9] Diabetes is a chronic morbid condition which requires lifelong treatment. So the cost of antidiabetic drug is the major deciding factor for the patients’ compliance. Selection of oral antidiabetic drugs as first-line drug or combined therapy should be based on both the pharmacological properties of the compounds like efficacy, safety profile and also on the clinical characteristics of the patient like stage of disease, body weight, BMI etc., There exists a wide range of variation in the prices of drugs marketed in India and other countries of the world. Percentage cost variation is an effective tool to find out the difference between the various brands prescribed by prescriber in the same setting. [10]
In 2005, Indian Council of Medical Research has given guidelines for treatment of diabetes in which the selection of drugs are mainly based on body mass index (BMI).
Judicious use of anti-diabetic drugs by adhering to these guidelines will decrease the complications and cost of the drug therapy. There are many studies carried out on drug utilization in diabetic patients but a limited number of studies had focus on analyses of cost and adherence to treatment guidelines.
So, we planned to carry out this study drug utilization studies in diabetic patient with focus on cost analyses and adherence to standard treatment guideline.
Objectives
To study prescription pattern, calculate cost of antidiabetic agents and to evaluate the adherence to treatment guidelines in diabetic patients attending the medicine outpatient department in a tertiary care teaching hospital.
Materials and Methods
A prospective, cross-sectional study was carried out over the duration of 5 months from October 2012 to February 2013. All the demographic data and complete prescriptions were collected on predesigned case record form. All the diabetic patients attending the medicine outdoor department were enrolled in the study after explaining the aim of the study. Written informed consent was obtained from each patient. Prior approval of Institutional ethics committee, hospital superintendent and from the head of the medicine department was obtained. Patients receiving any of the anti-diabetic drugs were included in the study irrespective of their gender and those patients who were pregnant and having insufficient data or records were excluded from the study. Anatomical therapeutic classification was used to designate each drug prescribed. [11]
Majority of drugs were prescribed by their brand names. For those prescriptions whose generic name of the drugs and price were not mentioned in the prescription, they were obtained from CIMS (current index of medical specialty) [12] and Indian drug review (IDR) [2012 issues]. [13]
We calculated the percentage cost variation this is an indicator of prescriber’s behavior.
We collected the patient’s pharmacy bills and analyzed the retail cost of a particular drug being manufactured by different companies, in the same strength, number and dosage form was compared. The difference in the maximum and minimum price of the same drug manufactured by different pharmaceutical companies was calculated. The drugs being manufactured by only one company or being manufactured by different companies however, in different strengths were excluded. Percentage cost variation was found out by using the following formula.
Percentage cost variation = 
For calculation of adherence to standard diabetes guidelines we used Indian Council of Medical Research Guidelines, 2005. [14]
Statistical analyses
All the data was entered in Microsoft Excel 2010®.The data was calculated using MYSTAT Software 12.0® and Statistical Package for Social Sciences Software 21.0 (SPSS)®. We used unpaired t-test and Fischer’s exact test to evaluate the difference between two groups. P value less than 0.05 was considered significant.
Results
A total of 250 prescriptions were collected in the study during the period of 5 months.
Highest numbers of the patients were found in the age group of 51-60 (36%) years. Out of the 250 patients 126 (50.4%) were male and 124 (49.6%) were female. The age difference between two gender groups (P ≤ 0.05) was statistically significant as shown in Table 1. Most common co-morbid condition was hypertension (100%).
| Variables | Gender | Mean±SD | P value |
|---|---|---|---|
| Age | Male | 59.49±8.79 | 0.007* |
| Female | 56.31±9.71 | ||
| Body mass index | Male | 27.16±2.85 | 0.066 |
| Female | 26.40±3.65 | ||
| Fasting blood glucose | Male | 115.85±31.46 | 0.480 |
| Female | 113.19±27.80 | ||
| Postprandial blood glucose | Male | 210.89±35.78 | 0.791 |
| Female | 209.5±46.92 | ||
| No. of drugs prescribed | Male | 5.59±2.48 | 0.8762 |
| Female | 5.54±2.59 | ||
| No. of anti-diabetic drugs prescribed | Male | 2.24±0.97 | 0.3684 |
| Female | 2.13±0.96 | ||
| Cost of anti-diabetic drug therapy | Male | 369±335.91 | 0.4390 |
| Female | 339±272.14 | ||
| Anti-diabetic drug combination used | Male | 0.648±0.52 | 0.3697 |
| Female | 0.59±0.50 |
*P≤0.05 by using unpaired t-test, no. of males=126 and no. of females=124
Table 1: Demographic variables (n=250)
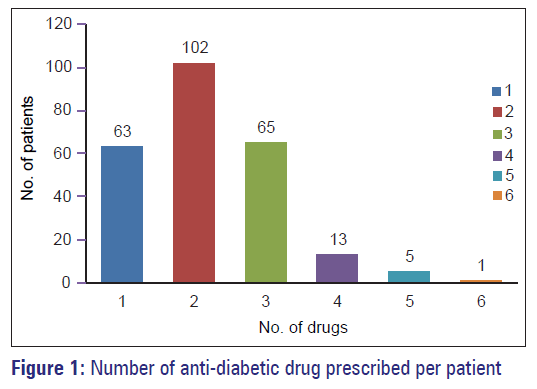
Number of drugs prescribed was 1,391 (Range 2-11). Number of drugs prescribed ranged from 2-14 drugs, with a mean of 5.56 ± 2.52 drugs. A total of 539 antidiabetic drugs were used as shown in Table 2 and Figure 1 (Range 1-6). Most commonly used drug was Metformin 218 (40.45%). Most common route used oral in 95.62% followed by subcutaneous route (11.32%). A total of 156 antidiabetic combinations were used. Most commonly used drug combination was of Glimepiride and Metformin in 119 (76.28%) patients. Most commonly used drugs other than antidiabetic were aspirin 146 (18.9%) and atorvastatin 119 (15.41%).
| ATC code | Class of anti-diabetic agents | Drugs (ATC code) | No. of patients* (%) |
|---|---|---|---|
| A10A Insulins and | A10AB Insulins | Insulin | 61 |
| analogues | and analogues for | (A10AB) | (11.32) |
| injection, fast-acting | |||
| A10B Blood | A10BA Biguanides | Metformin | 218 |
| glucose lowering | A10BAO2 | (40.45) | |
| drugs, excl. insulins | |||
| A10BB | Glimepiride | 153 | |
| Sulfonamides | A10BB12 | (28.39) | |
| Glibenclamide | 1 | ||
| A10BB01 | (0.19) | ||
| A10BX Meglitinides | Repaglinide | 10 | |
| A10BX02 | (1.86) | ||
| A10BF-Alpha | Voglibose | 51 | |
| glucosidase | A10BF03 | (9.46) | |
| inhibitors | |||
| A10BG | Pioglitazone | 29 | |
| Thiazolidinediones | A10BG03 | (5.38) | |
| A10BH-Dipeptidyl | Sitagliptin, | 9 | |
| peptidase 4 (DPP-4) | A10BH01 | (1.30) | |
| inhibitors | Vildagliptin | 2 | |
| A10BH02 | (0.37) |
*Many patients received more than one drug. ATC: Anatomical therapeutic chemical classification system
Table 2: Drug use pattern of anti-diabetic drugs (n=250)
In our study, therapy cost for a diabetic patient ranged from 15 to 2501 INR per month and most of the patients fall in the cost range of 100-400 INR i.e. in 68.4% of the patients. Mean cost of therapy for a diabetic patient was 354.60 ± 305.72 INR. Percentage cost variation is shown in Table 3 which ranges from 1.47 to 181.81 for Glimepiride + Metformin + Pioglitazone and glimepiride alone, respectively. WHO drug prescribing indicators are shown in Table 4 and adherence to ICMR guidelines on diabetes is shown in Table 5.
| Drugs | Percentage cost variation |
|---|---|
| Glimepiride+Metformin+Pioglitazone | 1.47 |
| Insulin | 20.49 |
| Voglibose | 31.43 |
| Pioglitazone+Metformin | 48.148 |
| Metformin | 123.08 |
| Glimepiride+Metformin | 127.78 |
| Glimepiride | 181.81 |
Table 3: Percentage cost variation of anti-diabetic agents
| Core indicator | Value |
|---|---|
| Average drugs prescribed | 5.57 |
| Generic name wise drug prescribed | 4.38% |
| Antibiotics used | 0.79% |
| Injections used | 4.38% |
| Drugs listed in (Essential Drug List)-India (2011) | 45.23% |
| Drug cost on injections | 4.38% |
| Average drug cost (Rs)/prescription | 866.63±617.64 Rs. |
Table 4: WHO Core prescribing indicators
| Body mass index | Total (%) | No. of prescriptions according to ICMR guidelines (%) | No. of prescriptions not following ICMR guidelines (%) | P value# |
|---|---|---|---|---|
| <18.5 | 1 (0.4) | 1 (0.4) | 0 (0) | 1.00 |
| 18.6-24.9 | 40 (16) | 38 (15.2) | 2 (0.8) | 0.035 |
| >25 | 209 (83.6) | 170 (68) | 39 (15.6) | 0.035 |
| Total | 250 | 209 (83.6) | 41 (16.4) |
*Many patients received more than one drug. ATC: Anatomical therapeutic chemical classification system
Table 5: Adherence of treatment to indian council of medical research guidelines, 2005
Discussion
This study was carried out with aim to analyze the drug utilization pattern in diabetic patients in medicine outpatient department in a tertiary care teaching hospital. Drug utilization research study will help for improvement in drug usage, more focused generic brand prescribing pattern. Selecting proper cost effective brand will help in quality of the drug usage, cost reduction, proper dose selection and better health outcome.
Diabetes is a chronic disease requiring a lifelong treatment. Although lifestyle modifications play an important role in diabetes management, drugs become unavoidable in many patients. This study was focusing on the prescription pattern in diabetic patients attending the outpatient departments in a hospital.
Two hundred and fifty patients were participated in our study. Demography details shows male patients were 126 (50.4%) and females patients were 124 (49.60%). In our study, male and female patients were almost equal in number. However in earlier study male predominance was seen in the study population which is not in agreement with the results of our study. [15] This may be due to difference in geographical location. Majority of 90 (36%) of the patients were found in 51-60 years of age group and among 43 (17.2%) newly diagnosed patients with Type-II DM, 30% were of the age group of 41-50 years indicating that the risk of type-II DM increases after the age of 40 years, this result was similar to study of Roy V et al (1998). [16] Middle age preponderance was seen in our study which was similar to an earlier study of Das P et al., (2011) were the patients ranged from 35-64 years. [17] Average age of male was 59 years and female was 56 years. It was reported in near to study of Wu et al. (1998). [18]
Average BMI observed in our study was 27.16 ± 2.85 in male patients and 26.40 ± 3.65 in female patients during course of antidiabetic therapy, which implies that the patients were overweight (BMI ≥ 25 kg/m2) and were on the borderline of becoming obese (BMI ≥ 30 kg/m2), which in itself is a well-recognized significant risk factor for diabetes mellitus. In our study, average FBS and PPBS notified was 113.19 ± 27.80 and 209.5 ± 46.92 mg/dl respectively in female and 115.85 ± 31.46 and 0.89 ± 35.78 mg/dl respectively in male. It was higher than that reported in the study done by Dave DJ et al. [19]
Hypertension and hyperlipidemia was the most common co-morbid condition associated with diabetes. Similar result was obtained by the study conducted by Rataboli P et al., (2007) stated that among all diabetic complications, cardiovascular complications (hypertension) pose a major threat. Hypertension accounted for 70.62% of the total complication. [20]
In our study, we also found out that the genetic basis i.e., majority of the patients had either of their parents suffering from diabetes mellitus this finding was further substantiated by study of Kannan et al., (2011) both showed positive genetic preponderance in diabetic patients. [1] Most of our patients had a history of diabetes around 5-15 years which an earlier study also reported. [21]
In our study, most commonly used drug group used was biguanides and sulfonylureas and not insulin as it was OPD based as compared to other studies. [7,22,23] The most common drug prescribed was metformin as compared to previous studies done a decade back. This suggests the gradual takeover of metformin as a first-line agent for type-2 DM in a decade. Among sulfonylureas, selection of glimepiride and glipizide has been recommended by Texas Diabetes Council because these agents have lower incidence of hypoglycemia. [1] Insulin was prescribed for 12% of patients with type 2 diabetes. Johnson JA et al. (2006) stated that a study from Spain reported that 25.3% of the patients were prescribed insulin. This difference is due to difference in presentation in different study populations. [24]
In this study it was found that combination therapy was more used than monotherapy. A total of 156 antidiabetic combinations were used. Most commonly used drug combination was of glimepiride and metformin which was a common finding seen with earlier study of V. Sivasankari et al., and Das P et al., (2011) which also suggest combination of biguanides and sulfonylureas was most frequently used combination and most effective one. This combination is most desirable and having a rational basis of use i.e. both of this drugs act through different mechanism one is insulin sensitizer and other insulin secretogogue. [7,17]
Most commonly used drug other than anti-diabetic drugs was aspirin, atorvastatin and clopidogrel which suggest association of cardiovascular disease especially hypertension and higher blood cholesterol level in diabetes mellitus patients. Whereas certain other drugs like pregabalin and mecobalamin were prescribed for patients having signs and symptoms of diabetic neuropathy.
Mean drugs prescribed per patient was 5.56 ± 2.52 whereas study by DasP et al., (2011) suggests Mean drugs prescribed per patient was 1.83. [17] Out of all drugs 619 (44.50%) antidiabetic drugs were prescribed which was a similar finding of an previous study conducted by Upadhyay D et al. (2007) where anti-diabetics accounted for 314 (45.84%) of the total drugs. [23] Average number of antidiabetic drugs per prescription was 1.45 which was similar to an early Indian studies. [1,22]
Our study and another study of Upadhyay D et al., (2007) reported that 95.62% of the drugs were prescribed in oral dosage form and only insulin was prescribed by parenteral route. This was a good prescribing habit to improve patient compliance. [23].
Data was analyzed for WHO drug utilization indicators, we have seen a trend of using brand name for prescribing and a very less amount of drugs was prescribed by generic names. More and more amount of drugs should be prescribed by generic names as it increases uniformity and decreases cost of drug therapy. In earlier study essential drugs were prescribed to a large extent but in our study nearly half numbers of drugs were prescribed from essential drug list which suggest a trend of using newer drugs in prescribing and also suggest the influence of pharmaceutical companies in prescribing.
A very less amount of drugs was given in injections as compared to earlier study. This finding can be explained as we collected only outpatient prescriptions and insulin was the most frequently prescribed drug by injection route which is a cornerstone of type 1 DM and also this also suggest better knowledge of the doctors about the risks and high cost of these injections. Only few antibiotics (0.79%) were prescribed out of all drugs it was an expected finding as patient in outpatient department arrives only for refilling of prescription and present mostly without infection. The percentage of generics and drug use from essential drug list are higher when compared to those from a study reported in Delhi by Kumar R et al (2013). [25]
Cost of therapy per month was higher as compared to study by Kannan et al. [1] Cost of drug therapy was a cause for non-adherence. In this study cost of the drugs per prescription was found to be very high. The cost of prescription can be reduced by choosing most economic drugs without changing its quality. Similar result was obtained by the study conducted by Kannan et al. [1]
Cost of prescription is important in chronic diseases like diabetes. In our study therapy cost for a diabetic patient ranged from 15 to 2501 INR and most of the patients fall in the cost range of 100-400 INR per month. Mean cost of therapy for a diabetic patient was 354.60 ± 305.72 INR, in our study it was found higher as expected as no anti-diabetic drug was given free of cost in our institute as compared to other government hospitals. [1]
We found out the percentage cost of variation an estimation of variability in cost for different brands prescribed to the patients. Glimepiride, Metformin and Pioglitazone combination had the least percentage cost variation i.e. 1.47 whereas Glimepiride had highest percentage cost variation i.e. 181.81, this finding suggest availability of more brands in Glimepiride as compared to other drugs and total cost of treatment can be reduced drastically by using the cheapest brand of Glimepiride and prescriber should avoid writing the costliest brand of glimepiride in order to curtail the total cost of drug therapy. Similar result was obtained by the study conducted by Jadhav NB et al. (2013) Stated that Glimepiride (1 mg) shows maximum price variation of 655.38%. [26]
ICMR guidelines have suggestion that in patient less than 18.5 Body Mass Index metformin should not be used, in patients in between 18.6 to 24.9 BMI guidelines suggest that metformin should be used as second line OAD only in the resistance cases after using other OAD and metformin should be combined when used. Whereas in patients above 25 BMI first-line drug used should be metformin. In our study majority (15.6%) of the non-adherence was due to prescribing of other drugs in place of metformin in the patients having BMI more than 25. Prescribing drugs other than metformin in inappropriate as literature showed that using in obese patient metformin should be preferred.
Conclusion
Metformin was the most commonly prescribed drug. Sulfonylurea and biguanide combination drugs were used. In these glimepiride and metformin combination drugs were prescribed and used commonly. Oral dosage form was the most commonly used to increase the patient compliance in type 2 DM. This is a good prescribing habit. In this study cost of drugs per prescription was found to be very high. The cost of prescription can be reduced by choosing the most economic drugs (generic) without changing its quality. Prescribers followed the ICMR guidelines to a large extent. The pattern of prescription for diabetic patients should be more rational as per our study and compliant with current evidence and clinical guidelines.
Acknowledgment
We are very grateful to Dr. Pankaj R. Patel, Dean of Smt. N.H.L. M.M.C who allowed us to complete this study.
References
- Kannan, Arshad, Senthil K. A study on drug utilization of oral hypoglycemic agents in Type-2 diabetic patients. Asian J Pharm Clin Res 2011;5:60-4.
- About Diabetes. Available from: http://www.who.int/diabetes/action_ online/basics/en/index.html [Last accessed on 2013 Jul 20].
- Day C. The rising tide of type 2 diabetes. Br J Diabetes Vasc Dis 2001;1:37.
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care 1998;21:1414-31.
- Chaudhari VP, Ganguly B. Changing pattern of prescribing antidiabetic agents in patients suffering from diabetes mellitus. Int J Basic Clin Pharmacol 2013;2:47-50.
- Hermansen K, Mortensen LS, Hermansen ML. Combining insulins with oral antidiabetic agents: Effect on hyperglycemic control, markers of cardiovascular risk and disease. Vasc Health Risk Manag 2008;4:561-74.
- Sivasankari V, Manivannan E, Priyadarsini SP. Drug utilization pattern of anti-diabetic drugs in a rural area of Tamilnadu, South India – A prospective, observational study. Int J Pharm Biol Sci 2013;4:514-9.
- Gama H. Drug utilization studies. Arq Med 2008;22:69-74.
- Karande S, Sankhe P, Kulkarni M. Patterns of prescription and drug dispensing. Indian J Pediatr 2005;72:117-21.
- Misra B, Jain SK, Mehta Y. A study on availability and prices of medicines in India. National Pharmaceutical Pricing Authority, 2002. Available from: http://nppaindia.nic.in/inde×1.html. [Last accessed on 2013 Jul 20].
- WHOCC-ATC/DDD Index. Available from: http://www.whocc.no/ atc_ddd_index/[Last accessed on 2013 Jul 20].
- CIMS-Asia. Available from: http://www.cimsasia.com/[Last accessed on 2013 Jul 20].
- Malik A, Malik S. Indian Drug Review Compendium. 1st ed. India: Mediworld Publications; 2012.
- Section 7. Pharmacological Treatment For Diabetes. ICMR Guidelines for Management of Type 2 Diabetes- 2005. Available from: icmr.nic.in/ guidelines_diabetes/section7.pdf [Last accessed on 2013 Jul 20].
- Abdi SA, Churi S, Kumar YS. Study of drug utilization pattern of antihyperglycemic agents in a South Indian tertiary care teaching hospital. Indian J Pharmacol 2012;44:210-4.
- Roy V, Rewari S. Ambiguous drug pricing: A physician’s dilemma. Indian J Pharmacol 1998;30:404-7.
- Das P, Das BP, Rauniar GP, Roy RK, Sharma SK. Drug utilization pattern and effectiveness analysis in diabetes mellitus at a tertiary care centre in Eastern Nepal. Indian J Physiol Pharmacol 2011;55:272-80.
- Wu SY, Lung BC, Chang S, Lee SC, Critchley JA, Chan JC. Evaluation of drug usage and expenditure in a hospital diabetes clinic. J Clin Pharm Ther 1998;23:49-56.
- Dave DJ, Dikshit RK, Gandhi AM. Utilization of some newer oral antidiabetic agents in a tertiary care hospital. Natl J Physiol Pharm Pharmacol 2012;2:146-51.
- Rataboli PV, Dang A. Antimicrobial price variation: Conundrum of medical profession. J Postgrad Med 2007;53:72-4.
- De Pablos-Velasco PL, Martinez-Martin FJ, Molero R, Rodriquez-Perez F, Puente G, Caballero A. Pattern of prescription of hypoglycemic drugs in Gran Canaria (Canary Islands, Spain) and estimation of the prevalence of diabetes mellitus. Diabetes Metab 2005;31:457-62.
- Sultana G, Kapur P, Aqil M, Alam MS, Pillai KK. Drug utilization of oral hypoglycemic agents in a university teaching hospital in India. J Clin Pharm Ther 2010;35:267-77.
- Upadhyay DK, Palaian S, Ravi Shankar P, Mishra P, Sah AK. Prescribing pattern in diabetic outpatients in a Tertiary Care Teaching Hospital in Nepal. J Clin Diagn Res 2007;3:248-55.
- Johnson JA, Pohar SL, Secnik K, Yurgin N, Hirji Z. Utilization of diabetes medication and cost of testing supplies in Saskatchewan, 2001. BMC Health Serv Res 2006;6:159.
- Kumar R, Kohli K, Kajal HL. A study of drug prescribing pattern and cost analysis among diabetic patients in a Care Teaching Institute in North India. J Drug Deliv Ther 2013;3:56-61.
- Jadhav NB, Adhav MSBCV. Cost analysis study of oral antidiabetic drugs available in Indian market. Int J Med Res Health Sci 2013;2:63-9.