Developing a Standard Treatment Protocol Towards Organophosphorus Poisoning for Emergency Department in a Hospital, India
Citation: Usha M, Satish Kumar BP, Shahin Maria J, Ebru Joseph S, Laxman W. Developing a Standard Treatment Protocol Towards Organophosphorus Poisoning for Emergency Department in a Hospital, India. J Basic Clin Pharma 2017;8:S64-71
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Background: Organophosphorous poisoning is one of the most common pesticide poisoning in India. Aim of this study is to develop standard treatment protocol to manage cases with a special reference of treatment practice from our tertiary care hospital and various literature resources. Methods: It was descriptive, observational, study conducted at rural tertiary care teaching hospital, within a time period of 6 months. Data were collected retrospectively and prospectively and were documented according to epidemiology, clinical characteristics and Treatment practices of different class of OP poisonings to develop standard treatment protocol for the future reference. Data were analysed using Microsoft excel. Results: Total of 150 patients; 100 retrospective and 50 are prospective. We found that males are more commonly poisoned. Majority of them were within age group of 20-30 years, farmer (62.66%), literate (62.66%), both alcoholic and smokers (52.33%). We also identified 28 different compounds where 11 such compounds were responsible for death (7.33%). It was already documented that there is no evidence of using pralidoxime to the compounds likes Dioxanthion, Phoxim, Propenofos and Prothiophos. There is an evidence of using Vitamin E and Magnesium sulphate for specific OP compounds. We formulated comprehensive guideline for each type of OP compound poisoning for our hospital for better patient care. Conclusion: Early identification of poison through clinical history, appropriate use of antidotes and decontamination procedure has to be reviewed in our hospital. Our guideline gives the insight to evidence based practice for management of OP poisoning.
Keywords
Organophosphorous poisoning, dioxanthion, phoxim, profenofos
Introduction
Poison is any substance, which obstructs with ordinary body functions and is capable of affecting adverse effects in living organisms. Poisoning can take place by means of ingestion, inhalation, or contact purposefully or accidentally that causes injury or damage to the body. The branch of medicine that deals with the study, diagnosis and management of poisons is known as toxicology. Poisoning is a main cause of morbidity and mortality globally. [1] Poisoning is the IVth most common cause of mortality in India predominantly in rural area as a result of a wide range of contributing factors. According to the World Health Organisation (WHO), globally more than three million of acute poisoning cases, with 0.3 million mortality occur annually. [2] Chemical poisons are classified into two groups that come into direct human contact (medications, cosmetics) and those that are not meant for human contact (household or domestic products, industrial products, agricultural pesticides, petroleum products, and non-pharmacological herbs). [2] The extent of damage depends on the amount of the poisonous material ingested and the amount of absorption and distribution, are depends on the innate power of the poison. [3]
World Health Organization (WHO) estimated that around 3 million pesticides poisoning arises globally and causes more than 22, 00,000 deaths annually [4] Insecticides and other agrochemical fertilizers are used to a greater magnitude and the poisoning with such products are more usually noticed in rural area. Many studies reveal that the Organophorous (OP) compounds constitute the most common poisoning agents. [5] Thousands of these compounds have been screened and over one hundred of them have been sold for this purpose. [6] Organophosphorus group of toxin occurred subsequently in the 19th century. The number of intoxications with Organophorous pesticides is estimated at some 30, 00,000 per year, and the number of deaths and causalities some 3,00,000 annually.
As the Organophosphorus poisoning are easily available and causes quick fatal action in minor doses when consumed, they are broadly used as suicidal poisons. [7] Death from unintended Organophosphorus poisoning are a less common than those from intentional poisoning and seems to be more common in regions where highly toxic Organophorous pesticides (WHO Class I toxicity) are available. Suicidal poisoning with OP compounds has increased incidence and carries 4-30% mortality in Indian studies. Most of the fatality rate is due to intentional poisoning by OP compounds, which has been reported in southern and central India.
The OP pesticides generally inhibit the carboxyl ester hydrolases, particularly acetyl cholinesterase (AChE) in human. Early identification followed by effective management in the initial stages increases the rate of existence among OP patients. Standard treatment includes initial gastrointestinal decontamination followed by intravenous administration of atropine and pralidoxime to inhibit acetyl cholinesterase. The role of atropine in OP poisoning is already well established. The benefits of Oximes are not clear in these patients. Several studies shows that the efficacy of oxime’s in OP poisoned patients are obtaining contradictory results about its efficacy. Most of the studies are not mentioned clearly either the dose of oxime or the severity of poisoned ingestion at the time of admission. Recently, glycopyrrolate has also been used as an alternative for atropine. [6]
Hospitals in rural regions bear the effect of this problem, seeing many hundreds of patients infected by insect repellent every year, with an incident mortality of 15-30%. [5] The suggestion for treatment in OP patient is pathetic and the confirmation use of the antidote is specific. Hence this study focuses to develop a standard treatment protocol towards Organophorous poisoning for the emergency department of Adichunchanagiri Hospital and Research Centre, B.G. Nagara.
Materials and Methods
Study design
This study was both retrospective and prospective observational disease focused descriptive study.
Study duration
The retrospective study was carried out over a period of 1 year from September 2014 to August 2015 and prospective study over a period of 6 months from September 2015 to march 2016.
Study site
The study was done in the Emergency department of Sri. Adichunchanagiri Hospital and Research Centre, B.G. Nagara and in the fertilizer shops of in and around B.G. Nagara.
Source of data and materials
WHO guidelines; Literature from fertilizer shops; Patient profile form; Patient case sheets.
Inclusion criteria
All inpatients ingested by Organophosphorus poisoning visiting during the study period. Patients who are willing to give consent.
Exclusion criteria
Patients with other poisoning where diagnosis about poisoning is not established.
Results and Discussion
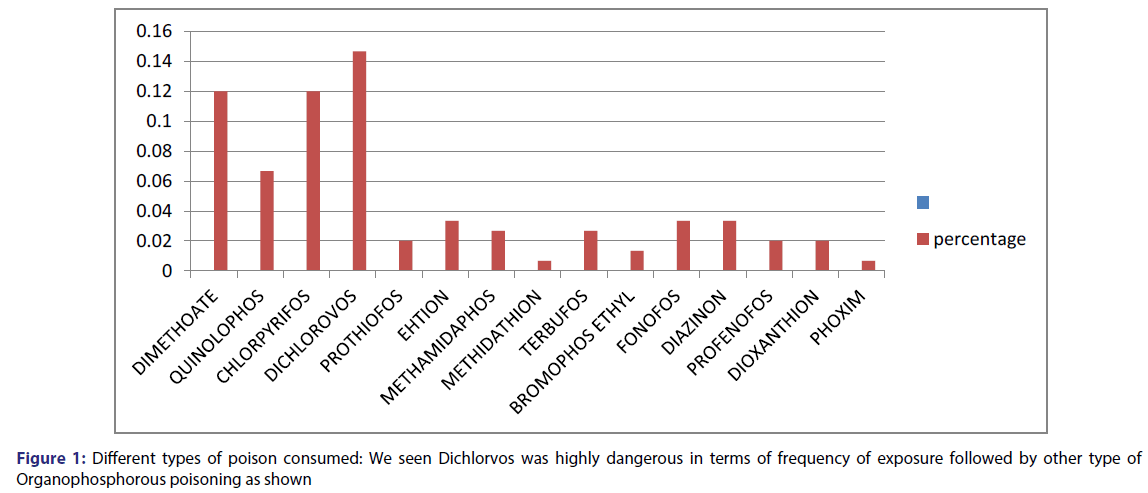
A total of 150 patients were included in our studies. Among them 100 retrospective and 50 prospective cases of Organophosphorus poisoning. Based on the study, we found following pattern of poisoning and treatment [Tables 1-3; Figure 1].
| Patient details | Retrospective Frequency (F1) | Prospective Frequency (F2) | Total frequency | Percentage (%) |
|---|---|---|---|---|
| Age group | ||||
| 10-20 | 14 | 2 | 16 | 10.66% |
| 20-30 | 36 | 23 | 59 | 39.33% |
| 30-40 | 24 | 12 | 36 | 24% |
| 40-50 | 13 | 6 | 19 | 12.6% |
| 50-60 | 8 | 2 | 10 | 6.66% |
| 60-70 | 5 | 5 | 10 | 6.66% |
| Gender distribution | ||||
| Female | 28 | 11 | 39 | 26% |
| Male | 72 | 39 | 111 | 74% |
| Occupation status | ||||
| Agriculture | 72 | 22 | 94 | 62.66% |
| Driver | 7 | 7 | 14 | 9.33% |
| Business | 14 | 7 | 21 | 14% |
| Carpenter | 1 | 0 | 1 | 0.66% |
| coconut climb | 1 | 0 | 1 | 0.66% |
| house wife | 20 | 8 | 28 | 18.6% |
| Not written | 9 | 0 | 9 | 6% |
| Student | 16 | 5 | 21 | 14% |
| water supply | 1 | 0 | 1 | 0.66% |
| Tailor | 0 | 1 | 1 | 0.66% |
| Social Habits | ||||
| Alcoholic | 8 | 11 | 19 | 12.66% |
| Smoker and alcoholic both | 21 | 17 | 38 | 25.33% |
| Smoker | 14 | 6 | 20 | 13.33% |
| Not smoker and alcoholic | 57 | 16 | 73 | 48.66% |
| Education status | ||||
| Literate | 59 | 35 | 94 | 62.66% |
| Illiterate | 41 | 15 | 56 | 37.33% |
| Total | 100 | 50 | 150 | 100% |
Table 1: Demographic Details of Patient.
| Clinical characteristics of patients Arrival at hospital after exposure | Retrospective Frequency (F1) | Prospective Frequency(F2) | Total frequency | Percentage (%) |
|---|---|---|---|---|
| <1 | 33 | 10 | 43 | 28.66% |
| 2-3 hr | 4 | 5 | 9 | 6% |
| 3-4 hr | 7 | 7 | 14 | 9.33% |
| 4-5 hr | 17 | 11 | 28 | 18.66% |
| 5-6 hr | 24 | 12 | 36 | 24% |
| 6-7 hr | 4 | 1 | 5 | 3.33% |
| 7-8 hr | 2 | 1 | 3 | 2% |
| 8-9 hr | 8 | 1 | 9 | 6% |
| 9-10 hr | 1 | 2 | 3 | 2% |
| Mode of exposure | ||||
| Accidental | 9 | 8 | 17 | 11.33% |
| Impulsive | 31 | 41 | 72 | 48% |
| Intention | 60 | 1 | 61 | 40.66% |
| Place of exposure | ||||
| Field | 23 | 18 | 41 | 27.33% |
| Home | 64 | 24 | 88 | 58.66% |
| Market | 6 | 7 | 13 | 8.66% |
| Others | 7 | 1 | 8 | 5.33% |
| Time of exposure | ||||
| Morning (10 am-12 pm) | 3 | 7 | 10 | 6.66% |
| Afternoon (12 pm-5 pm) | 27 | 21 | 48 | 32% |
| Evening (5 pm-10 pm) | 16 | 11 | 27 | 18% |
| Night (10 pm-12 am) | 4 | 5 | 9 | 6% |
| Midnight (12 am-6 am) | 27 | 1 | 28 | 18.66% |
| Early morning (6 am -10 am) | 33 | 5 | 38 | 25.33% |
| Reason of poisoning | ||||
| Accident | 6 | 1 | 7 | 4.66% |
| Alcohol dependent syndrome | 4 | 0 | 4 | 2.66% |
| Back pain | 1 | 0 | 1 | 0.66% |
| Business loss | 11 | 3 | 14 | 9.33% |
| Depression | 11 | 4 | 15 | 10% |
| Exam failure | 8 | 3 | 11 | 7.33% |
| Family problem | 12 | 14 | 26 | 17.33% |
| Financial crisis | 2 | 0 | 2 | 1.33% |
| Job issues | 1 | 0 | 1 | 0.66% |
| Love failure | 1 | 0 | 1 | 0.66% |
| Loan repay | 6 | 4 | 10 | 6.66% |
| Marriatalconflict | 3 | 0 | 3 | 2% |
| Abdominal pain | 1 | 0 | 1 | 0.66% |
| Property issues | 10 | 10 | 20 | 13.33% |
| Quarrel | 23 | 11 | 34 | 22.66% |
| Outcome of patient | ||||
| Death | 6 | 5 | 11 | 7.33% |
| Recovered | 94 | 45 | 139 | 92.66% |
Table 2: Clinical Characteristics of Poisoned Patient
| Patient demographic of fatal case | Prospective | Retrospective | Frequency | Percentage (%) |
|---|---|---|---|---|
| Occupation | ||||
| Agriculture | 3 | 1 | 4 | 36.36% |
| Business | 0 | 2 | 2 | 18.18% |
| Student | 0 | 2 | 2 | 18.18% |
| House wife | 1 | 1 | 2 | 18.12% |
| Driver | 1 | 0 | 1 | 9.09% |
| Age group | ||||
| 10-20 | 0 | 2 | 2 | 18.18% |
| 20-30 | 1 | 2 | 3 | 27.27% |
| 30-40 | 1 | 1 | 2 | 18.18% |
| 50-60 | 1 | 1 | 2 | 18.18% |
| 60-70 | 2 | 0 | 2 | 18.18% |
| Gender | ||||
| Male | 4 | 3 | 7 | 63.63% |
| Female | 1 | 3 | 4 | 36.37% |
Table 3: Demographic of fatal cases
Discussion
Organophosphorus (OP) compounds first synthesized in early 1800s were developed as insecticides in early 1900s and found world wide application by 1941. During the 1930s, pesticide research led to the synthesis of numerous organophosphorus compounds. [8-10]
In this current work we found lots of OP compounds owing to different groups are available here in India for poisoning. We found intoxication by these agents is increasing. We also found different reason where, when, why, how and which set of population is getting more exposure to these compounds in our society. We also observed the changing pattern of poisoning every year considering both retrospective and prospective data. Resuscitation, decontamination, early use of specific antidote, close observation and good supportive care were all the basis of management in our study. Despite large number of studies worldwide, the current evidence base on management is small. Text books recommend varied therapeutic antidote regimens leading to controversies and confusion. Considering these things in mind we tried to develop standard treatment guideline for our setting.
To develop a guideline we followed basically following three steps
1. Describe the epidemiology of OP poisoning of our hospital and also to detect change in pattern of exposure per year, it is based on retrospective and prospective data.
2. Identify and discuss the treatment practice of OP poisoning of our tertiary care centre.
3. On the basis of findings of our study and with the help of literature resources we offer comphrensive treatment protocol.
Demographic Information of Poisonous Patients
We found males were frequently poisoned with Organophosphorus compound in our village in comparison with female. This trend is similar to Dhaval et al. study. [11] But it is contrast to the study done by Kora et al. [12] and Pokhrel et al. [13] where they found female were more poisoned.
It shows that male and female both can be predominant in terms of exposure. Considering the age group of poisonous patient; mostly population within the age group of 20-30 year is being affected followed by 30-40 age groups and 40-50 age groups. Elderly group 60-70 and age group between 10-20 is also poisoned but in very less extent. Padmanabha et al. also seen majority of the victims were in the age group of 21-30 years which is similar to our setting. It may be because this age group was the most active one, physically, mentally and socially and so, it was more prone to stress during life, also for family problems, love failure, unemployment, failure in examination, etc. Based on retrospective and prospective data there is similar trend of age group and gender exposure every year.
Stratification of poisonous patient based on occupation showed mostly people from agricultural background were poisoned and trend of exposure every year is similar. They either do not know how to use these agents as pesticide or becoming easily accessible for intentional poisoning. Some were business man, driver, carpenter, coconut climber, tailor, student, house wife etc. Exposure to poison for student is decreasing. These people who had poisoned were also using drugs of social abuse like alcohol, cigarettes (52%) etc. It is also interesting to note that most of the people were literate (62.66%) in our study.
Time of consumption of poison
Out of 150 cases, 48 (32%) cases were intoxicated with OP compound during afternoon time between 12 pm to 5 pm which was similar to studies done by Sinha et al., Emerson et al. and Maharani et al. But it is contradictory to study done by Pokhrel et al. in which the incidence was high during night time. Trend analysis showed that in previous year mostly people took poison at early morning (6 am-10 am) i.e., 33/150 patient but this year trend had changed to afternoon.
Time of arrival, between intake of poison and arrival to hospital
The time interval between the intake of the poison and the attendance by a doctor is very important for outcome of these patients. Previous year people came to our hospital within a time period less than 1 hr but this year we had seen some delay i.e., after 5-6 hr. The later result is almost similar in Dash et al. [13] Overall people arrive in hospital less than 1 hr (28.66%) and then within 5-6 hr (24%) followed by within 4-5 hr. The mortality rate will directly depend on the time at which the patient receives the treatment.
Place, mode and reason of exposure to poison
Majority of patient (58.66%) found home as safe place to take poison whereas other majority i.e., 27% directly took poison or get exposed accidently in their field. In very less extent some took poison in market place where they bought and get access the poison. (8.66%).
In our study; overall mode of exposure is impulsive (48%) other than intentional (40.66%) and accidental (11.33%). It is however that more number of people intentionally took poison in previous year comparison to this year. Reason for all this was many. Quarrel>business>loss>de pression>property issues>exam failure>accident>loan pay>alcohol abuse and dependence>marital conflict>financial crises>back pain>job issues>love failure>abdominal pain, were all the reason in previous year to take the poison but in this year family problem followed by quarrel>property issues>loan pay>depression>exam failure>business loss>accident, were most prominent cause of poisoning.
Outcome of poisonous patients
The mortality rate in the present study was 7.33% i.e., 11 out of 150 cases died which was similar to study by Padmanabha et al. [12] where he found mortality rate was 8.77% in their study. In contrast Sahin [14] and Kora [10] studies had found very less mortality in comparison to our study. We also found similar mortality rates every year. Stratification of death cases based on age showed that 20-30 age groups were more prominent. Mostly their occupation was agriculture, student and some sort of business. We also noted that most of this patient came after at least 4 hr of the exposure and stayed in hospital for at least 6 days, minimum 1 day to maximum 17 days.
Type of OP compounds
We had seen 13 different OP compounds responsible for poisoning near our village. Most frequent exposure took place by Dichlorovos i.e., 16.66% but it didn’t cause any mortality. It is however that, it extends the length of hospitalization. Quinalophos, Chlorpyrifos, Phoxim, Diazinon, Methidathion, Terbufos, and Dimethoate were responsible for 8 deaths of poisonous patients in our study. Monocrotophos is class I toxic pesticides available in local market. These compounds caused death owing with early and rapid onset of respiratory paralysis within few hours of ingestion. [15-18]
Identification of pesticide
Firstly, identification of pesticide at admission is very important to know. In our study, identification is done through history given by patient, container of pesticide and clinical presentation. We observed 53.33% of patient provided clinical history, 20% patient presented with container and 100% came with clinical feature of cholinergic excess having spectrum of nicotinic, muscarinic and CNS features. Additional strategy for early identification of pesticide in cases when patient with not clear history of exposure is needed in our hospital. It is because Carbamate poisoning also cause cholinergic excess and can be easily confused with OP poisoning. Asking patients to identify pesticide by making and showing photographs of pesticides available in the local market will help in this instance. WHO colour code on container can give clue further. In case of disparity between history and clinical presentation it is recommended to follow clinician own clinical judgement. Acetylcholine esterases and pseudo cholinesterase essays are also used in our centre to confirm either these pesticide eliminated from body or not. But these essays are less specific to identify pesticide and takes time to perform, so it should be avoided for identification purpose.
Initial stabilization: Emergency and supportive measures
Acute severe organophosphorus pesticides poisoning is a medical emergency. In our hospital; emergency measures involved maintenance of an open airway and assisted ventilation, especially after extensive skin exposure or ingestion of a highly fat soluble agents were followed. Treatment ensures that the patient had a patent airway and adequate breathing and circulation Oxygen was provided at the first opportunity. However, little evidence supports the common advice that the atropine must not be given until oxygen is available. In hospitals that have no access to oxygen, atropine can be given early to patients with pesticides poisoning to reduce secretions and improve respiratory function. The patient should be placed in the left lateral position, with the neck extended. This position reduces risk of aspiration; helps keep the airway patent, and could decreases pyloric emptying and absorption of poison. In our hospital supportive care aimed for giving fluids and control of blood glucose etc.
Gastrointestinal decontamination
Gastric lavage was the first intervention poisoned patients received on presentation to our hospital. 90% of patient’s undergone lavage and skin decontamination simultaneously where as some people undergone emesis also (2.66%). Some patients (5.33%) underwent only lavage. No evidence shows any form of gastric decontamination to benefit patients poisoned with Organophosphorous. Gastric decontamination should only be done after the patient has been stabilized and treated with Oxygen, Atropine and Oxime. Guidelines for treatment of drug self – poisoning suggest that lavage should be considered only if the patient arrives within 1 hour of ingesting poison.
Ipecacuanhainduced emesis should not be used in organophosphorus pesticide poisoning. Patients poisoned with Organophorous can rapidly become unconscious, rising aspiration if ipecacuanha has been given. Mechanically-induced emesis with large quantities of water risks pushing fluid through the pylorus and into the small bowel, probably increasing the rate of absorption. No evidence suggests that patients with pesticide poisoning benefit from treatment with activated charcoal.
Antidotes and other drugs used for OP poisoning
As antidote Atropine, Glycopyrrolate and Pralidoxime were used in our hospital. Apart from antidotes, different drugs were used for different indication like Protein powder as protein supplement, Insulin to control Blood glucose, Multivitamin for weakness, Antibiotics as prophylaxis, Antidiarrheal to treat diarrhoea possibly due to antibiotic or poison, Benzodiazepines to treat agitation and tremor symptom, Antiemetic to treat vomiting, Proton pump inhibitors and Histamine receptor 2 blockers to decrease gastric mucosa erosion and IV. Fluids for dehydration and maintain homeostasis.
OP compound specific treatment protocol
Dimethoate:
| 1. | First aid | Gastric lavage with 5%sodium bicarbonate may be given, if swallowed. Wash contaminated skin and irrigate eyes with normal saline. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg, at 5-10 min interval for hours. The need for further atropine administration is indicated by the continuous of symptoms as much as 25-50 mg, atropine may be required in a day. Dissolve 1-2 gm, of PAM in 10 ml distilled water and inject intravenously very slowly for 10-15 minutes. |
Quinolophos:
| 1. | First aid | Remove the patient to fresh air. Induce vomiting by tickling the back of the throat. Wash contaminated skin with soap and water. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval for hours together. The need for further atropine administration is indicated by the continuance of symptoms. As much as 25-50 mg may be required in a day. The extent of salivation is a useful criterion to follow in adjusting the dosage of atropine. Administer 1-2 gm of 2-PAM diluted in 10cc of distilled water and injected intravenously very slowly taking 10-15 minutes. |
Chlorpyrifos
| 1. | First aid | Remove the patient to fresh air. Induce vomiting by tickling the back of the throat. Wash contaminated skin with soap and water. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval for hours together. The need for further atropine administration is indicated by the continuance of symptoms. As much as 25-50 mg may be required in a day. The extent of salivation is a useful criterion to follow in adjusting the dosage of atropine. Administer 1-2 gm of 2-p.a.m diluted in 10cc of distilled water and injected intravenously very slowly taking 10-15 min. |
Dichlorvas
| 1. | First aid | Move the exposed person to fresh air at once. If breathing has stopped, perform artificial respiration. Keep the affected person warm and at rest. Immediately wash the contaminated skin using soap or mild detergent and water. If the person is conscious, give large quantities of water immediately. Try to get the person to vomit by having him touch the back of his throat with his finger. Wash eyes immediately with large amounts of water, lifting the lower and upper lids occasionally. Contact lenses should not be worn when working with this chemical. |
| 2. | Drug therapy | Administer atropine sulfate intravenously, or intramuscularly, if iv injection is not possible. In moderately severe poisoning: adult dosage: 0.4-2.0 mg repeated every 15 minutes until atropinisation is achieved: tachycardia (pulse of 140 per minute), flushing, dry mouth, dilated pupils). Maintain atropinisation by repeated doses for 2-12 hours or longer depending on severity of poisoning. Dosage for children under 12 years: 0.05 mg/kg body weight, repeated every 15 minutes until atropinisation is achieved. Maintain atropinisation with repeated dosage of 0.02-0.05 mg/kg. In severely poisoned individual may exhibit remarkable tolerance to atropine; two or more times the dosages suggested above may be needed. Administer in cases of severe poisoning in which respiratory depression, muscle weakness and twitching are severe. Adult dosage: 1.0 gm intravenously at no more than 0.5 gm per minute. Child's dose (under 12 years): 20-50 mg/kg (depending on severity of poisoning) intravenously, injecting no more than half the total dose per minute. Dosage of pralidoxime may be repeated in 1-2 hours, then at 10-12 hour intervals if needed. In very severe poisonings, dosage rates may be doubled. |
Profenofos:
| 1. | First aid | Give 1 or 2 glasses of water and induce vomiting by touching back of throat with finger. Do not induce vomiting or give anything by mouth to an unconscious or convulsing person. Wash thoroughly with soap and water and get medical attention immediately. If in eyes flush with plenty of water for at least 15 minutes and get medical attention. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval until continuance of symptoms. There was no apparent response to oxime therapy. |
Prothiofos:
| 1. | First aid | Gastric lavage is done with normal saline. In case of eyes and skin contact, flush with plenty of clean water. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval until continuance of symptoms. There was no apparent response to oxime therapy. Oximes are less effective in ethyl compounds. |
Ethion:
| 1. | First aid | Treatment must ensure that the patient has a patent airway and adequate breathing and circulation. Ideally, oxygen should be provided at the first priority. The patient should be placed in the left lateral position, with the neck extended. This position reduces risk of aspiration; helps keep the airway patent, and could decrease pyloric emptying and absorption of poison. Supportive care should include giving fluids and control of blood glucose. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval until continuance of symptoms. Administer 1-2 gm of 2-p.a.m diluted in 10cc of distilled water and injected intravenously very slowly taking 10-15 min Vitamin E is recommended in Ethion poisoning. |
Terbufos:
| 1. | First aid | Oxygen was given immediately with the monitoring of clinical respiratory effort of poisons pulse oximetry and arterial blood gas if respiratory distress was present. Check airway, breathing, and circulation. Place patient in the left lateral position, preferably with head lower than the feet, to reduce risk of aspiration of stomach contents. Skin decontamination and gastric lavage should be done. |
| 2. | Drug therapy | Administer intravenous access and give 1–3 mg of atropine as a bolus, depending on severity. Set up an infusion of 0·9% normal saline; Aim to keep the systolic blood pressure above 80 mm Hg and urine output above 0.5 ml/kg/h. Record pulse rate, blood pressure, pupil size, presence of sweat, and auscultator findings at time of first atropine dose. Administer pralidoxime chloride 2 g (or Obidoxime 250 mg) intravenously over 20–30 min into a second cannula; follow with an infusion of pralidoxime 0·5–1 g/h (or Obidoxime 30 mg/hr) in 0·9% normal saline. 5 min after giving atropine check pulse, blood pressure, pupil size, sweat, and chest sounds. If no improvement has taken place, give double the original dose of atropine. If seizure occurs administer Diazepam i.v. |
Fonofos:
| 1. | First aid | Provide high flow oxygen, if available. Intubate the patient if their airway or breathing is compromised. The clothes should be removed and the skin vigorously washed with soap and water. People involved in first aid should wear rubber gloves so as to prevent skin absorption of the poison. Gastric lavage may help to reduce the absorption of the ingested poison and should be considered in patients presenting within 1-2 hours of ingestion of poison. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval until continuance of symptoms. PAM was given intermittently every 8th hour for 3-4 days and atropine as a continuous infusion which help in maintaining constant plasma concentration of the drug. Glycopyrrolate also used in patients which reduced the atropine requirement in the patients. Glycopyrrolate in combination with atropine reduces the atropine toxicity and also improves the quality of treatment. |
Methamidophos:
| 1. | First aid | Provide high flow oxygen, if available. Intubate the patient if their airway or breathing is compromised. The clothes should be removed and the skin vigorously washed with soap and water. Gastric lavage is done with in 1 hour after ingestion. |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval until continuance of symptoms. Pralidoxime should be administered intravenously at 30 mg/kg initially over 30 min, followed by constant infusion of 8 mg/kg/hr in dextrose 5% solution. It could be continued until the full recovery or until atropine is required. Benzodiazepines to protect against central nervous system seizures. |
Diazinon:
| 1. | First aid | Do not make an unconscious person vomit. Wear protective gloves when administering first aid. Gastric lavage procedure can be undertaken within 60 minutes of ingestion. |
| 2. | Drug therapy | Administer intravenous access and give 1-3 mg of atropine as a bolus, depending on severity. Administer 1-2 gm of 2-P.A.M diluted in 10cc of distilled water and injected intravenously very slowly taking 10-15 min. Intravenous magnesium sulfate in a dose of 4 g only on the first day after admission was recommended. Infusion of high doses of sodium bicarbonate (5 meq/kg in 60 min. Followed by 5-6 meq/kg/day to obtain arterial blood ph of 7.45 to 7.55). |
Bromophos ethyl:
| 1. | First aid | Provide high flow oxygen, if available. Intubate the patient if their airway or breathing is compromised. The clothes should be removed and the skin vigorously washed with soap and water. Gastric lavage is done with in 1 hour after ingestion |
| 2. | Drug therapy | Atropinise the patient immediately and maintain full atropinisation by repeated doses of 2-4 mg at 5-10 min interval until continuance of symptoms. For children, the doses are 0.04-0.08 mg of atropine/kg body weight Administer 1-2 gm of 2-P.A.M diluted in 10cc of distilled water and injected intravenously very slowly taking 10-15 min. Magnesium therapy in addition to atropine and Oximes has been found to benefit. |
Conclusion
Organophosphorous poisonings is the most common poisoning admissions that require intensive care admission and management and is a prime reason for the visit to the emergency department. The high incidence of suicide by poisoning among young adults can be checked by frequent psychological counselling and by tackling their problems sympathetically.
Majority of the study population was prescribed with antidote in a combination (Atropine+Pralidoxime). Most of the time the treatment has been done symptomatically so that the clinical presentations have been taken in to consideration. Inappropriate prescription of drugs (broad spectrum antibiotics) by the physicians accelerated the emergence of drug resistance, especially in case of antibiotics prescription.
Resuscitation, decontamination, early use of specific antidote, close observation and good supportive care were all the basis of management in our study. Majority of the patients recovered which indicates good emergency and intensive care management at this hospital. Despite large number of studies worldwide, the current evidence base on management is small. Prevailing treatment protocols require updating on proper guidelines, counselling and training programs for the health care professionals which may help to reduce the mortality and morbidity rate due to the poisoning.
Acknowledgements
We would like to acknowledge B. Ramesh, principal of Sri Adichunchanagiri College of pharmacy and all physician of emergency department of our institutional hospital.
REFERENCES
- Shivaramu MG, Vijay Kumar AG, Kumar U. A Comprehensive Analysis of Poisoning Case in Rural Area: A Retrospective Autopsy Study. Scholars Journal of Applied Medical Sciences 2015;3:565-7.
- Siva S, Reddy TM, Ahammad SF, Durga Prasad TS. Pattern Of Acute Poisoning, Therapeutic Approach And Outcomes In South Indian Tertiary Care Teaching Hospital, Andhra Pradesh. International Journal of Universal Pharmacy and Biosciences 2015:67-8.
- Goel A, Aggarwal P. The National Medical Journal of India 2007;20:1-16.
- Eddleston M, Buckley AN, Eyer P, Dawson HA. Management of Acute Organophosphorus Pesticide Poisoning. Lancet 2008;371:597-607.
- Shakuntala S, Yogesh G. Analysis of Organophosphorus Poisoning at Tertiary Care Hospital: A Report. Journal of Evidence Based Medicine and Healthcare 2015;2:421-30.
- Nurulain MS. Different Approaches To Acute Organophosphorus Poison Treatment, Department of Pharmacology and Therapeutics. FMHS, UAE University 2012;42:712-7.
- Palaniappen V. Current Concepts in the Management of Organophosphorus Compound Poisoning, pp: 427-33.
- Eddleston M. Early management after self-poisoning with an Organophosphorus or Carbamate pesticide a treatment protocol. 2004;8:391-7.
- Buckley NA. Speed of initial atropinisation in significant Organophosphorus pesticide poisoning a systemic comparison of recommended regimens. J Toxicol Clin Toxicol 2006;46:865-75.
- Lin TJ. Epidemiology of organophosphate pesticide in Taiwan. Clinical toxicology. Taylor and Francis Online 2008;46:1-3.
- Yelmos F, Diez F. Acute organophosphate pesticide poisoning in the province of Almeria, A study of 187 cases. Europe PubMed Central 2015:1-2.
- Buckley NA, Eddleston M, Szinicz L. Oximes for acute organophosphate pesticide poisoning. Cochrane Database System Rev 2005.
- Paudyal BP. Organophosphorus poisoning. J Nepal Medicine Association 2008;47:251-8.
- Buckley NA, Eddleston M, Dawson AH. The need for translational research on antidotes for pesticides poisoning, US National Library of Medicine National Institute of Health. PubMed 2005.
- Aardama H, Meertens JHJM, Ligtenberg JJM, Peters Polman M, Tullenken JE. Organophosphorus pesticide poisoning cases and developments. The Journal of Medicine 2008;66:149-53.
- Sundaray NK, Ratheesh KJ. Organophosphorus poisoning: Current management guidelines. Medicine Update 2010;20:420-5.
- Kumar MR. A retrospective analysis of acute Organophosphorus poisoning cases admitted to the tertiary care teaching hospital in south India. 2014;13:71-5.
- Krupesh N, Chandrashekar TR, Ashok AC. Organophosphorus poisoning- still a challenging proposition. Indian Journal of Anaesthesia 2002;46:40-3.