Assessment of Asthma Treatment Outcomes among Adult Outpatients at Nemmh Chest Clinic in Hadiya Zone, Southern Ethiopia
- *Corresponding Author:
- Ramanjireddy Tatiparthi
Assistant Professor, School of Pharmacy, Institute of Health Sciences, Jimma University, Jimma, Ethiopia.
E-mail: ramanjireddy.brahmareddy@ju.edu.et
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: Asthma is one of the chronic inflammatory disorder of the airways in which many cells and cellular elements play a major role. It is an estimated about 344 million people have the condition as per global asthma network in 2014. The progress of the disease is getting downhill in particular in quickly developing countries, as Ethiopia is one of the east Africa’s fast developing country as evidenced by its GDP improvement. The estimated prevalence of asthma in Ethiopia is about 9.1% as per Global asthma network. So, This study aims to assess the asthma treatment outcomes among the adult patients on follow-up at NEMMH, Southern Ethiopia. Methods: A retrospective study was designed and conducted based on the asthma patient information card at NEMMH for the past two years (Jan 1st 2014-Jan 1st 2016 G.C). The collected data were analyzed by using SPSS software. Results: A total of 174 asthmatic patient’s cards was reviewed, and among the patients majority (62.6%) were male and the mean age of the respondents was 35.1 years with standard deviation (SD) of 9.4. The most (53.45%) used asthma drug combination was Salbutamol with Prednisolone for long term asthma control. Among the patients, 40.8% were prescribed for antibiotics for their respiratory and urinary tract infections. The study found that there is a strong effect of social drug abuse with disease improvement (p-value<0.05). Conclusion: This study has demonstrated that despite the availability of effective therapy for asthma, the control of disease is sub-optimal and it falls short of the standard treatment guidelines set by the global network.
Keywords
Asthma, retrospective study, exacerbations, outcomes, Ethiopia
Introduction
Background of the study
In 2014, the global asthma network reported the prevalence of asthma is intensifying in industrialized developing countries, approximately 334 million people estimated to have this condition which increased from 300 million asthma patients were in 2006. Although most of the countries started the new guideline strategies against the asthma, It is still in aggravation and throws the challenges in reducing the morbidity and mortality rates. The rates remain high, with an estimated as per Disability Adjusted Life Presence of more years lost (DALYS) of 15 million/year and Years of Life lost to disease (YLD) of 2.2%. [1,2]
Since we know much about the asthma, it is a chronic inflammatory disorder of the airways highly associated with airway hyper responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing, in most cases, the diagnosis of asthma was delayed due to the confusion between the symptoms of asthma with pneumonia. [3] The progress and severity of the disease can be measured by asthma control test, it is based on 5 symptoms survey that assess the activity, shortness of breath, nocturnal symptom, rescue medication use and self- rating of asthma patient. [4]
Airborne substances, pollen, dust mites, mold spores, animal wastes, smoking, physical exercise can cause the asthma, one of the atypical asthma is occupational asthma is due to farming, painting, cleaning work, and plastic manufacturing. Over 300 substances causes the asthma conditions, they are highly reactive molecules, some of them are isocyanines, platinum salts, animal biological products that stimulate the production of IgE. [5]
There was a suggestion that current and past smoking were related to a higher risk of emergency department visits. Compared with never smoking, current smoking was prospectively associated with a greater risk of hospitalization and hospital-based care for asthma as well as affecting treatment outcome. Cigarette smoking could increase the severity of asthma by accelerating the loss of lung function that typically accompanies asthma. Cigarette smoking may also reduce the responsiveness to inhaled corticosteroids, the cornerstone of controller therapy for asthma. [6]
Individual patients also respond in various ways to different classes of medications for asthma, including inhaled corticosteroids, leukotriene modifiers, and beta-adrenergic agonists. Because of the inherent variability in responses to therapy, many patients remain symptomatic despite close adherence to national asthma education and prevention program (NAEPP) guidelines. [7] These guidelines adopted a stepped care approach to intensify the treatment with asthma severity. With the least awareness of the NAEPP guidelines, the asthma is still poorly controlled due to patients and physician’s non adherence. [3]
In Canada, asthma remains poorly controlled in nearly 60% of patients, which places an excess burden on the health care system, and accounts for between 250-300 deaths per year. [8] It identified that there was an inappropriate medication use. More than 40% of the patients didn’t receive a prescription of inhaled corticosteroids, which is the mainstay of asthma control, according to NHI (Nursing and Homemakers Inc) guidelines. [9]
Symptom rates are lower than in industrialized countries, while only South Africa approaches rates found in the UK. Rural African regions always showed much lower asthma prevalence rates than urban areas. [10,11]
Many asthmatics in Nigeria are treated symptomatically with only oral bronchodilators such as Salbutamol and aminophyline – usually under self supervision. [12]
Asthma prevalence in eastern Africa, including Eretria, Somalia, Kenya is estimated at 4.4%, most of prescribers not following the asthma management guidelines. If it comes to Ethiopia the prevalence rate was 9.1% as per an article published in PLOS medicine asthma in Africa, and if we come to an area of our study in southern Ethiopia is Hawassa estimated about 4.3% for those living in 270 kilometers away from its capital city, Addis Ababa where it was 11.4% this may due to industrialization. [13,14]
Most international asthma management guidelines recommend that patients initially diagnosed with asthma receive short acting beta2 agonist (SABA), preferably by inhalation, combined with inhaled steroids. If poor response is noted, the patient should be prescribed a long acting beta2 agonist (LABA), combined with inhaled steroids. Other add-on medications may include like leukotriene receptor antagonists, theophyllines. During exacerbations, the patients should receive systemic steroids, nebulizer SABA and oxygen until the patient is stable. [15]
Even though there is much data is available worldwide, there are few literatures on asthma in Ethiopia. Therefore, the aim of this study is to assess asthma treatment outcomes among adult patients, who followed up at a NEMMH chest clinic in Hadiya zone, southern Ethiopia. This study will pave the way to tackle situations of irrational use of asthma drugs conforming to GINA and Ethiopia’s standard treatment guidelines. This study is to identify the commonly prescribed anti– asthmatic drugs, find out the treatment outcomes and its association with independent variables.
Operational definitions
Severe asthma exacerbation- defined as a deterioration in asthma resulting in admission to hospital or visits the emergency department or requires systemic steroids for at least 3 days.
Mild asthma exacerbation- the occurrence of one of the following; using of two or more inhalations of as needed reliever in addition to the baseline 24 hour or morning PEF less than the baseline by at least 20% or night awaking due to asthma.
Well controlled asthma - is defined as asthma symptoms twice per week or less, a rescue bronchodilators medication used twice weekly or less, where is no nocturnal or early morning waking, no limitations of work and exercise, the patient and their physicians consider well controlled asthma.
Poorly controlled asthma- is defined as when the patient has at least one reported hospitalization due to asthma or high frequency of symptoms in the last year.
Materials and Methods
Study design and population
A retrospective cross sectional study was conducted at NEMM Hospital based on the asthmatic patient’s card information available past two years from 1st Jan 2014 to 1st Jan 2016 G.C. This study area can be found in Hosanna town located 232 km southern direction away from the capital city of Ethiopia, Addis Ababa. The study was conducted from 10th Jan to 28th Jan, 2016 G.C. All 174 asthmatic patients treated for asthma were selected on a systematic random sampling for this study and their patient cards were reviewed.
Criteria’s for inclusion and exclusion
Inclusion criteria’s
All patients greater than or equal to 18 years.
Patients who have been on follow-up for the last two years.
Exclusion criteria’s
Those patients who have started treatment less than a month.
Those patients who have incomplete asthmatic patient profile form (medical record).
Variables of the study
Dependent variables
Prescribing pattern: Asthma Medications and Concurrent medication
Treatment outcome: Asthma exacerbation and Asthma related hospitalization
Independent Variables
Age, Sex, Marital status, Patient characteristics, occupation, social drug use
Data collection and processing
Data collection tools
The checklist/data collection format was adapted after reviews of different literatures. Necessary correction was adopted after reviewing of patient profile card that is pertinent to the study.
Data collection and data quality assurance
Data was collected by the data collectors. All selected outpatient cards of asthmatic patient were reviewed and the result was evaluated according to the guidelines of GINA. Pretest was conducted to avoid the errors in the collection. On receipt of every day, data were checked for consistency in response. Ethical clearance letters of permission were presented to NEMM Hospital office and verbal consent was received prior to the study upon agreement of privacy maintenance with the patient information.
Results
Socio-demographic characteristics of asthmatic patients
From a total of 174 subjects, the majority (62.6%) of them were male and the remaining 37.4% were female asthmatic patients, the mean age of the respondents was 35.1 years with a standard deviation (SD) of 9.4, most were between 55-64 years accounted 37.3%. This result indicated that, large numbers were elder patients. In regard to the residence of the respondents 113 (65%) were from rural and 61 (35%) were urban. Out of the total asthmatic patients, majority 126 (72.4%) of the patients were married followed by 38 (21.3%) single, 6 (4%) divorced and 4 (2.3%) of treated patients were widowed. The type of occupation that treated patients engaged was shown that 31.03% patients were employees in governmental and private institutions, 23.56% were engaged in agricultural sector, 15.5% were housewives, 14.4% of treated patients engaged in business sectors like trade/commerce and piety trade and 9.8% were students in different level. The remaining 5.4% of treated patients engaged in other occupations like religious works, laborers.
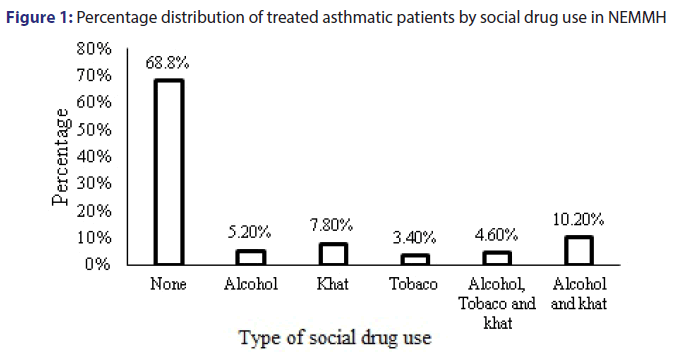
Of the total patients, as Figure 1 shown that the significant number of patients identified as not users of any form of social drugs like khat, alcohol, cigarette. etc., whereas, 10.2% were using both alcohol and khat users, 7.8% were using khat only, 5.2% were using alcohol only, 4.6% were using all alcohol, tobacco and cigarettes and the remaining 3.4% were using tobacco only in the study period.
Clinical characteristics of asthmatic patients
During the two year period of study, 59% were having an asthma exacerbation among patients, whereas 41% were with no asthma exacerbation among patients. Only 25% of patients were hospitalized minimum in once in their follow up due to asthma related symptoms, the majority (60.2%) patients were hospitalized other than asthma symptom related cases whereas, the remaining 14.71% were due both to the causes.
As shown in Tables 1 and 2 below, shortness of breath is the most asthma symptoms manifested by the studied asthma patients during their visit. Wheezing was high during the first two visits (61.90%, 12, and 38%) respectively and low during the other patient visit. Chest tightness is the lowest asthma symptom manifested starting from the second visit.
| Asthma symptom | 1st visit | 2nd visit | 3rd visit | 4th visit | 5th visit |
|---|---|---|---|---|---|
| Symptom free | 25(11.9) | 63(30) | 103(49) | 118(56.2) | 140(66.5) |
| Wheezing | 130(61.90) | 26(12.38) | 19(9.04) | 23(10.95) | 24(11.43) |
| Cough | 151(71.90) | 115(54.76) | 74(35.24) | 72(34.28) | 47(22.38) |
| SOB | 172(81.91) | 120(57.14) | 63(30) | 45(21.42) | 55(26.19) |
| Chest tightness | 68(32.38) | 23(10.95) | 22(10.48) | 20(9.25) | 2(2.85) |
Table 1: Symptoms that manifested among asthmatic patients in NEMMH
| Asthma medication | Frequency (%) |
|---|---|
| SABA and prednisolone | 93(53.45) |
| SABA and beclomethasone puff | 40(22.98) |
| SABA, beclomethasone puff and prednisolone | 27(15.51) |
| SABA (Salbutamol puff and salbutamol tab) only | 14(8) |
| Total | 174(100) |
Table 2: The combination of anti- asthmatic drugs among asthmatic patient at NEMMH, at Hadiya zone, southern Ethiopia (2014-2016)
Asthma drug prescription pattern among the asthmatic patients
The most commonly prescribed anti-asthmatic drugs among the total asthmatic patients, 93 (53.45%) received were SABA (Salbutamol) with Prednisolone. The second prescribed combination therapy was SABA and beclomethasone puffs 40 (22.98%). No drug was prescribed as monotherapy.
Out of 174 studied asthmatic patients, 46 (26.4%) of them had no concurrent medication prescribed. Of the total concurrent medication prescribed, can be see in Table 3 antibiotics account 40.8%. Next to antibiotics, the most prescribed medications were drugs for dyspepsia, GERD and GI ulcer (antacid, omeprazole and cimetidine) which accounts 13.2%. According to NEMMH patient card record and follow up chart (2014-2016), some antibiotic used by patients include doxycycline, ceftriaxone, anti-TB, Augmentin, clarithromycin, azithromycin, erythromycin, metronidazole, chloramphenicol, amoxicillin, crystalline penicillin. Whereas, drugs for GERD and dyspepsia includes antacid, omeprazole and cimetidine. Cardiac medications includespironolactone, digoxin, HCT, lovastatin, propranolol, furosemide, enalapril. Anti-pain medication includes ASA, diclofenac, paracetamol and ibuprofen. Dermatological products includecloderm, calamine lotion, dexamethasone cream and Vaseline. Anti-histamine includes loratidine and citrizen. CNS drugs: amitriptyline. Anti- thyroid. Of 174 asthmatic patients, 54 (31.03%) of them uses SABA twice per week. The mean days of SABA use per week was detrmined as 3.09 (± 1.504).
| Concurrent medications | Frequency (%) |
|---|---|
| No concurrent medication | 46(26.4) |
| Antibiotics | 71(40.8) |
| Drugs for GERD and dyspepsia | 23(13.2) |
| Cardiac medications | 12(6.9) |
| Anti-pain medication | 7(4) |
| Dermatological drugs | 7(4) |
| Anti-histamines | 3(1.7) |
| CNS drugs | 3(1.7) |
| Anti-thyroid drugs | 2(1.15) |
Table 3: Concurrent medication prescribed among asthmatic patient at a chest clinic of NEMMH
Association between treatment outcome and selected factors
From 174 studied asthmatic patients, 56.2% were having poorly controlled asthma while the rest were controlled asthma 43.8%. There is a strong association between asthma exacerbation and occupational status and social drug use (p-value=<0.05) among the asthmatic patient shown in Table 4.
| Characteristics | Asthma exacerbation | Total% | p-value | ||
|---|---|---|---|---|---|
| Status | Yes (%) | No (%) | |||
| Sex | Male | 69(39.6) | 40(22.9) | 109(62.6) | >0.05 |
| Female | 34(19.5) | 31(17.8) | 65(37.4) | ||
| Age (years) | 18-24 | 7(4) | 2(1.15) | 9(5.2) | >0.05 |
| 25-34 | 11(6.3) | 2(3.5) | 17(9.78) | ||
| 35-44 | 18(10.3) | 13(7.5) | 31(17.9) | ||
| 45-54 | 9(5.2) | 1(0.6) | 10(5.7) | ||
| 55-64 | 49(28.2) | 16(9.2) | 65(37.3) | ||
| >64 years | 26(14.9) | 16(9.2) | 42(24.2) | ||
| Occupational status | Farmer | 35(20.1) | 6(3.5) | 41(23.56) | <0.05 |
| Student | 5(2.9) | 12(6.9) | 17(9.8) | ||
| Housewife | 21(12.1) | 6(3.5) | 27(15.5) | ||
| Employed | 34(19.5) | 20(11.5) | 54(31.3) | ||
| Merchant | 12(6.9) | 13(7.5) | 25(14.4) | ||
| Social drug use | None | 47(27) | 31(17.8) | 78(44.8) | <0.05 |
| Alcohol only | 15(8.6) | 8(4.6) | 23(13.2) | ||
| Chat only | 16(9.2) | 8(4.6) | 24(13.8) | ||
| tobacco only | 6(3.4) | 0 | 6(3.4) | ||
| Alcohol, tobacco and chat | 7(4) | 1(0.58) | 8(4.6) | ||
| Alcohol and chat | 25(14.4) | 10(5.7) | 35(20.2) | ||
Table 4: Cross-tabulation of association between asthma exacerbation and socio-demographic characteristics among asthmatic patients at NEMMH
There is no association between treatment outcome and sex and age of asthmatic patients since, the p>0.05 and there is a significance, association between treatment outcome and occupation of patients, and social drug use (p<0.05) shown in Table 5.
| Characteristics | Status | Treatment outcome | p-value | ||
|---|---|---|---|---|---|
| Poorly controlled asthma (%) | Well controlled asthma (%) | N=174 N (%) |
|||
| Sex | Male | 64(36.8) | 45(25.9) | 109(62.6) | >0.05 |
| Female | 34(19.5) | 31(17.8) | 65(37.4) | ||
| Age (years) | 18-24 | 6(3.4) | 3(1.7) | 9(5.2) | >0.05 |
| 25-34 | 13(7.5) | 4(2.2) | 17(9.78) | ||
| 35-44 | 20(11.5) | 11(6.4) | 31(17.9) | ||
| 45-54 | 8(4.6) | 2(1.1) | 10(5.7) | ||
| 55-64 | 42(24.1) | 23(13.2) | 65(37.3) | ||
| >64 years | 28(16.1) | 14(8.1) | 42(24.2) | ||
| Occupational status | Farmer | 29(16.7) | 12(6.8) | 41(23.56) | >0.05 |
| Student | 9(5.17) | 8(4.6) | 17(9.8) | ||
| Housewife | 19(10.9) | 8(4.6) | 27(15.5) | ||
| Employed | 37(21.3) | 17(9.9) | 54(31.3) | ||
| Merchant | 14(8) | 11(6.3) | 25(14.4) | ||
| Social drug use | Not using drug | 31(17.8) | 47(27) | 78(44.8) | <0.05 |
| Alcohol only | 18(10.3) | 5(2.9) | 23(13.2) | ||
| Chat only | 13(7.5) | 11(6.3) | 24(13.8) | ||
| tobacco only | 6(3.4) | 0 | 6(3.4) | ||
| Alcohol, tobacco and chat | 6(3.4) | 2(1.15) | 8(4.6) | ||
| Alcohol and chat | 27(15.5) | 8(4.6) | 35(20.2) | ||
Table 5: Cross-tabulation of association between asthma treatment outcome and socio-demographic characteristics among asthmatic patient at NEMMH
Discussion
Most of the patients diagnosed with asthma were in the 55-64 age groups (37.3) and male to female ratio was 2:1. This is inconsistent with findings done in Uganda in central Africa. In an asthma study in Spain and Latin America, which was found that 37.5% of the patients were in the 45-64 age group and 72% were females. [16-18] This might be due to geographical and occupational variability between the continents.
In this study, 25% of asthmatic patients’ precipitants for asthma exacerbation were lower and upper respiratory infection. This was supported by the study done in the United States which found that 22% of the patients with acute asthma were treated with an antibiotic. This suggests that the most precipitating diseases are infection related. This might be due to only limited patients who demonstrated to have bacterial LRTI received antibiotics as most cases of LRTI are viral. [19]
Despite the guideline recommends, 8% of the patients were routinely used only SABA either in tablets or inhalation dosage forms for the long-term control of asthma. This is lower than compared with the result of the studies done in Nigeria (57%). [20]
The most asthma drug combination is SABA+Prednisolone in which 53.45% of patients received for long term asthma control. This is higher than with the study done in Nigeria in which 41% of the patients took oral corticosteroid for long term asthma control. [17] This might be due to the high cost of inhaled corticosteroids (ICS)and poor adherence of physicians to the guideline.
ICS is currently the most effective anti-inflammatory medications for the treatment of persistent asthma. Studies have demonstrated their efficacy in the long-term management of persistent asthma. [11] Only 38.49% of patients used ICS combination with another drug in this study. This low utilization of inhaled steroids is supported by data from studies in Nigeria which is 28%. [18] In contrast with GINA guideline, there was no patient using ICS+LABA or LABA only. This low utilization of ICS mighty is due to poor adherence to standard treatment guidelines.
In this study, it was found that found that 40.8% patients were prescribed for antibiotics for management of upper and lower respiratory and urinary tract infection. This was supported by the studies done in the United States for which 22% of patients with acute asthma were treated with an antibiotic. This might be due to only limited patients who demonstrated to have bacterial LRTI received antibiotics as most cases of LRTI are viral.
The types of medication used for asthma therapy and Co morbid and precipitating diseases are the major determinant of treatment outcome. This study has demonstrated that despite the availability of effective therapy for asthma, the control of asthma is sub-optimal among asthma patients follow at NEMMH and falls short of the GINA guideline recommendations. 56.2% of the patients had poorly controlled asthma. The result of this study is inconsistent with data from previous surveys in a survey of asthma patients in Uyo, Nigeria observed poor control among 80% of the patients with a significant association between under-utilization of ICS and the use of systemic steroids with uncontrolled asthma. [18]
Gender, marital status, age and occupation have no association with treatment outcome, but there is an association between social drug use and treatment outcome (p-value <0.05) which is similar to studies conducted in England. [21]
Limitation of the study
This study has notable limitations. First, the retrospective nature of the study limited us to examine factors that predict outcome variables in a robust manner. Second, we did not investigate factors that were predictors for poor asthma symptom control.
Conclusion and Recommendation
Shortness of breath is the most asthma symptoms manifested by the studied asthma patients during their visit. Wheezing was high during the first two visits. Between the combination of anti- asthmatic drugs short acting B-agonist and Prednisolone was the most combinations. Of asthmatic patients, a use of SABA was twice per week.
More than half of the patient’s symptoms were poorly controlled. This study has demonstrated that despite the availability of effective therapy for asthma, the control of asthma is sub-optimal among the studied asthmatic patients, and falls in short of the standard treatment guidelines including the Ethiopian recommendations. Based on the key findings of this study, the following key points are recommended for improvement of asthmatic patients’ outcome treatment in the study area;-
• Resources should be channeled the patients on current recommendations of asthma management so as to improve the quality of life of the patients.
• The physician should record asthma symptoms, daily rescue medication use, and the duration of the medication given by the patients each visit appropriately.
• All asthma patients to follow up should be on chronic therapy of inhaled corticosteroid. Long acting B- blocker should be combined with an inhaled corticosteroid for long term control of asthma symptom.
References
- The Global Asthma Report 2014. Auckland, New Zealand: Global Asthma Network. 2014;16-8.
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet 2013;380:2197-223.
- Holgate ST, Polosa R. The mechanisms, diagnosis, and management of severe asthma in adults. The Lancet 2006;368:780-93.
- Abdelhamid E, Awad A, Gismallah A. Evaluation of a hospital pharmacy-based pharmaceutical care services for asthma patients. Pharmacy Practice (Internet) 2008;6:25-32.
- Koshak EA. Classification of asthma according to revised 2006 GINA: Evolution from severity to control. Annals of thoracic medicine 2007;2:45.
- Eisner MD, Iribarren C. The influence of cigarette smoking on adult asthma outcomes. Nicotine& tobacco research 2007;9:53-6.
- Fuhlbrigge AL, Adams RJ, Guilbert TW, Grant E, Lozano P, Janson SL, et al. The burden of asthma in the United States: level and distribution are dependent on interpretation of the national asthma education and prevention program guidelines. American journal of respiratory and critical care medicine 2002;166:1044-9.
- Bacon SL, Bouchard A, Loucks EB, Lavoie KL. Individual-level socioeconomic status is associated with worse asthma morbidity in patients with asthma. Respiratory research 2009;10:1.
- Juniper EF, Bousquet J, Abetz L, Bateman ED. Goal Committee. Identifying ‘well-controlled’ and ‘not well-controlled’ asthma using the Asthma Control Questionnaire. Respiratory medicine 2006;100:616-21.
- Odhiambo JA, Mungai MW, Gicheha CM, Nyamwaya JK, Karimi F, Macklem PT, et al. Urban- rural differences in questionnaire-derived markers of asthma in Kenyan school children. European Respiratory Journal. 1998;12:1105-12.
- Bereznicki BJ, Norton LC, Beggs SA, Gee P, Bereznicki LR. Review of the management of childhood asthma in Tasmania. Journal of paediatrics and child health 2013;49:678-83.
- Desalu OO, Fawibe AE, Salami AK. Assessment of the level of asthma control among adult patients in two tertiary care centers in Nigeria. Journal of Asthma 2012;49:765-72.
- Wjst M, Boakye D. Asthma in Africa. PLoS Med 2007;4:e72.
- Melaku K, Berhane Y. Prevalence of wheeze and asthma related symptoms among school children in Addis Ababa, Ethiopia. Ethiopian medical journal 1999;37:247-54.
- Bousquet J, Mantzouranis E, Cruz AA, Aït-Khaled N, Baena-Cagnani CE, Bleecker ER, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. Journal of Allergy and Clinical Immunology. 2010;126:926-38.
- Kirenga JB, Okot-Nwang M. The proportion of asthma and patterns of asthma medications prescriptions among adult patients in the chest, accident and emergency units of a tertiary health care facility in Uganda. African health sciences 2012;12:48-53.
- Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O’Byrne P, Barnes PJ, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. New England Journal of Medicine 1997;337:1405-11.
- Liou A, Grubb JR, Schechtman KB, Hamilos DL. Causative and contributive factors to asthma severity and patterns of medication use in patients seeking specialized asthma care. CHEST Journal 2003;124:1781-8.
- Stewart KA, Higgins PC, McLaughlin CG, Williams TV, Granger E, Croghan TW. Differences in prevalence, treatment, and outcomes of asthma among a diverse population of children with equal access to care: findings from a study in the military health system. Archives of pediatrics & adolescent medicine 2010;164:720-6.
- Umoh VA, Ekott JU, Ekwere M, Ekpo O. Asthma control among patients in Uyo South-Eastern Nigeria. Indian Journal of Allergy, Asthma and Immunology 2013;27:27.
- Aldington S, Beasley R. Asthma exacerbations. 5: Assessment and management of severe asthma in adults in hospital. Thorax 2007;62:447-58.