A Prospective Observational Study on Pattern, Severity and Outcome of Different Poisoning Cases in a Tertiary Care Hospital, India
Citation: Mate VH, Dhande PP, Gonarkar SB, Pandit VA. A Prospective Observational Study on Pattern, Severity and Outcome of Different Poisoning Cases in a Tertiary Care Hospital, India. J Basic Clin Pharma 2017;8:154-157.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Introduction: The severity and outcome in poisoning cases are determined by multiple factors including poison characteristics, mode and amount of poisoning as well as treatment opportunity.
Methods: This is a prospective observational study conducted in emergency medicine department of a tertiary care hospital. The study included 88 poisoning and 11 snake bite cases. Data regarding demographics, mode of poisoning, lag time in treatment, first aid, outside and indoor treatment, co-morbid illness, duration of hospitalization and final outcome were collected in a pre-structured proforma. Logistic regression and univariate analysis were used to predict the effect of different variables on the outcome by using Mann-Whitney U/Fisher’s Exact test. All the analyses were carried out using SPSS (version 18.0).
Results: Incidence of poisoning and snakebites had a preponderance of males(p<0.001). Majority of poisonings were organophosphorus compounds and alcohol intoxication. Duration of hospital stay reduced in patients who had less lag time in reaching the hospital (p=0.032) whereas higher Poison Severity Score (PSS)(p<0.001) and code blue activation(p<0.001) prolonged hospital stay. Chances of survival increased with early blue code activation(p<0.001) and worsened with higher PSS(p<0.001) and more lag time (p<0.014).
Conclusion: OP compounds and alcoholic intoxication were the most common poisons. Provision for reducing lag time and early treatment at initial stage of poisoning or snake bite is effective in reducing duration of hospitalization and possibly mortality. Educational and awareness programs, establishment of poison information and surveillance centers and regulations on pesticides/drug availability will form important strategies for the prevention of these emergencies.
Keywords
Poisoning, PSS, outcome, tertiary care hospital
Introduction
Poison is defined as any substance which when introduced into the living body or brought in contact with any part thereof will produce ill effects or death by its local or systemic action or both. [1] A case of poisoning is also defined as the overdose of drugs, medicaments and biological substances and/or a wrong substance given or taken in error (T36-T50, International Statistical Classification of Diseases and Related Health Problems–10th Revision (ICD-10). A case is considered as snake bite on the basis of history and presentation. Poisonings and snake bites constitute a major cause of hospitalization and mortality in developed as well as developing nations. The severity and outcome in such cases are determined by a number of factors such as chemical and physical properties of the poison, amount consumed, mode of poisoning, preexisting disease and most importantly treatment initiation. Pesticides are the most common cause of self-poisoning world wide, [2] (from 4% in the European region to over 50% in the Western Pacific region). [3] In a previous retrospective study from South India, organophosphorus compounds (OPC) were reported as the most common cause of poisoning (36.0%). [4] Another study from North India also reported OPC and Celphos (Aluminium Phosphide) as the most common poisonings. [5-7] Snake bite is also a major problem worldwide. The huge burden of poisoning and snake bite cases demands comprehensive strategies for reducing deaths. Hence, this prospective observational study was conducted with an aim to identify factors related to outcomes and to suggest strategies to reduce associated morbidity and mortality.
Material and Methods
This prospective, observational study was conducted after getting approval from Institutional Ethics Committee. Study was initiated in the emergency medicine department/casualty of tertiary care hospital. The patients were followed up in ICU/medicine ward. Study was carried out from April-Sept 2014. The patients who were brought dead or died immediately upon arrival before receiving any indoor treatment were excluded. Data collection form, designed by Pharmacology department of the institute was used for the study which comprised of demographic details of the patient, the time of poisoning/snake bite, time of hospital arrival, lag time in reaching the hospital, mode of transportation, mode of poisoning (accidental/suicidal/homicidal), history of First aid received, indoor treatment, door-to-needle time (defined as time from hospital arrival to administration of first treatment), antidote given, etc. “Code Blue” is generally used to indicate a patient requiring resuscitation or otherwise in need of immediate medical attention. [4] A standardized scale for grading the severity of poisoning allows qualitative evaluation of Morbidity caused by poisoning. Poison Severity Score was used as a tool for the study.
Statistical analysis
The results were expressed as percentage and mean ± standard deviation. Comparison of normally distributed numeric variables between groups was done using unpaired t-test. Logistic regression and univariate analysis were used to predict the effect of different variables on the outcome by using Mann-Whitney U/Fisher’s exact test. All the analyses were carried out using SPSS version 18.0. p-value <0.05 was considered statistically significant.
Results
Demographic details
Out of total 99 enrolled cases, poisoning were 88 and snake bites were 11. Mean age of the patients was 31 years although age was ranging from 2-78 yrs. Poisoning and snake bites were common (33.3%) in the younger (31-40 years) age groups with male preponderance (72%) (p<0.001) [Table 1].
| Characteristics | Number (%) |
|---|---|
| Poisonings | 88 (88.8) |
| Snake bites | 11 (11.2) |
| Gender | |
| Males | 71 (71.8 %) |
| Female | 28 (28.2%) |
| Marital status | 77 married (77.7%) |
| Residence | |
| Urban | 51 (51.5%) |
| Rural | 48 (48.5%) |
| Educational Qualification | |
| Illiterate | 2 (2) |
| Schooling | 36 (36.3) |
| College | 30 (30.3) |
| Graduate | 29 (29.2) |
| Postgraduate | 2 (2) |
| Occupation | |
| Business | 4 (4) |
| Government job | 2 (2) |
| Private job | 42 (42.4) |
| Farmer | 15 (15.1) |
| Student | 16 (16.1) |
| Housewife | 16 (16.1) |
| Others | 2 (2) |
| Co-morbid condition present | 34(34.4%) |
Table 1: Demographic details of poisoning cases
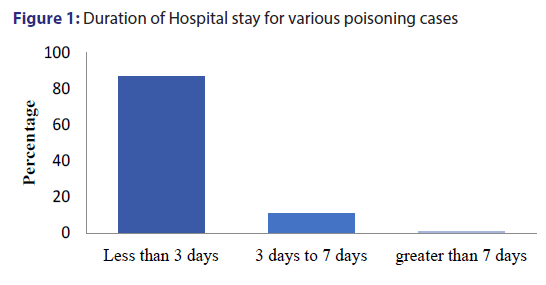
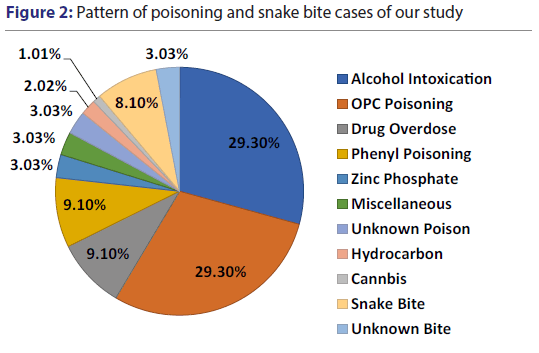
Figure 1 shows that 87.9% of these poisoning patients had less than 3 days hospital stay. As seen in the Figure 2, major types of poisonings included Organo-phosphorus compound (OPC) (29.3%), Alcohol Intoxication (29.3%), Phenyl poisoning (9.1%), Drug overdose (9.1%), Zink Phosphate (3.03%), etc. There were total 9 cases of drug overdose out of which 6 patients were of Alprazolam overdose. Also, 11 snake bite cases were found during the study period which have been included.
First aid
First aid in the form of induction of vomiting, removal of clothes, washing patient with water was given in 24% patients of Poisoning. First aid was given mainly by relatives in 18 patients and First contact physicians [1 MBBS and 2 AYUSH (Ayurveda, Unani, Siddha and Homeopathy) doctors] as well in 3 patients. Out of 11 snake bite cases, 8 patients (72.2%) received first aid treatment in the form of application of tourniquet.
Median lag time
The median lag time for hospital arrival in poisoning and snake bite cases was 120 and 90 minutes respectively. Transportation was the major problem for prolonged lag time in 74% of poisoning and 64% of snake bite cases. The mode of transportation was by personal/private vehicles (76.8%) or by ambulance (23.2%).
Mode of poisoning
The proportion of accidental cases was substantial (51.5%) and almost similar to suicidal cases (47.5%).
Outside treatment
59 patients (52 poisoning, 7 snake bites) received primary treatment outside tertiary care hospital by 20 MBBS and 39 AYUSH doctors. It was mainly in the form of lavage, intravenous fluids, injectable antibiotics, etc. None of the snake bite patient had received polyvalent anti snake venom. Of the other poisoning cases, 48% and 27% patients received Atropine and Pralidoxime as an antidote to OPC respectively. Out of 59 patients, who received outside treatment, only 4 patients died.
Door to needle time
The median door to needle time was 9.62 and 10.9 min in poisoning and snake bite cases, respectively.
Indoor treatment
Polyvalent anti-snake venom was given in 37.5% snake bite patients in the tertiary care hospital. Amongst all the poisoning cases, only 39% patients received treatment with antidote. Atropine, being the major drug to reverse the cholinergic symptoms, was prescribed to all patients with OPC poisonings. Antidote Pralidoxime was prescribed in 18/29 patients of OPC poisoning. One case of unknown poisoning and zinc phosphide poisoning also received atropine and Pralidoxime. Ethanol was given to all 3 patients of methanol poisoning.
Effect of various factors on patient outcome, duration of hospital stay and nature of poisoning
For outcome of poisoning, factors like age, sex, marital status, comorbid conditions, nature of poisoning, outside treatment, first aid did not show any statistically significant results as shown in Table 2.
| B | SE | Wald | Df | Sig | Exp (B) | 95% CI | p | |
|---|---|---|---|---|---|---|---|---|
| Age (Years) | -0.086 | 0.047 | 3.381 | 1 | 0.066 | 0.918 | 0.837 | 1.00 |
| Sex (M/F) | -0.489 | 1.043 | 0.220 | 1 | 0.639 | 0.613 | 0.079 | 4.73 |
| Outside T/t | -0.384 | 1.142 | 0.113 | 1 | 0.737 | 0.681 | 0.073 | 6.38 |
| Lag time (min) | 0.002 | 0.004 | 0.384 | 1 | 0.536 | 1.002 | 0.995 | 1.00 |
| Door to needle time | -0.349 | 0.191 | 3.349 | 1 | 0.67 | 0.705 | 0.485 | 1.02 |
| Constant | 2.856 | 3.469 | 0.678 | 1 | 0.410 | 17.398 |
Table 2: Logistic regression analysis of poisoning patients for outcome
Outcome vs. Code blue activation
Out of 13 patients in whom Code Blue was activated, 46% patients died and 54% patients survived. 86 patients in whom Code Blue was not activated, survival rate was 100% [Fisher exact test; p<0.001].
Outcome vs. PSS
In 94% of the patients who showed PSS score <2, the survival rate was 100%, while in rest of the patients where PSS score was >2 death rate was 100% (Mann-Whitney test; p<0.001).
Outcome vs. Lag time
Median lag-time in dead patients was 385 minutes as compared to 120 minutes in survived patients which shows statistically significant difference (Mann-Whitney test; p<0.014)
Nature of poisoning vs. door to needle time
For poisoning patients, mean door to needle time was 9.34 minutes and for snake bite cases 11.82 minutes (p=0.01).
Nature of poisoning and lag time in reaching to hospital
No statistical significance (p=0.18) was found between nature of poisoning and lag time in reaching to hospital although median lag time for poisoning was 120 minutes and for snake bites 90 minutes.
Nature of Poisoning and treatment reached outside the hospital
No significance (p=0.99) was observed between nature of Poisoning and treatment reached outside the hospital.
Discussion
The important objective of the study was to assess the pattern, severity and outcome of poisoning cases in a tertiary care hospital and measures to modify or improve outcome and hospital stay in poisoning and snake bite cases.
Our study revealed that poisoning and snake bites are very common in males (71.8%) [Table 1]. This finding is similar to that of other studies. [8-10] The high incidence of poisoning in males may be because of the high exposure to stress and strain and also because of insecticide poisoning occurring due to inappropriate handling Studies done in Japan and Turkey showed female had more preponderance. [11,12] Common age group affected was 12-40 years of age. Poisoning in this younger group may be due to less education, instability in life, insecure feeling, inability to accept failure, peer pressure, etc.
Almost 88% of poisoning and snake bite patients were admitted in tertiary care hospital for 1-3 days as seen in Figure 1. Most of the patients in whom code blue was not activated were hospitalized for less period as these patients may not be serious. Patients showing more PSS score were hospitalized for more period as there was wide spread involvement of various systems of the body.
As seen in Figure 2, common pattern of poisoning was OPC, Alcohol Intoxication, snake bites, Phenyl poisoning and drug overdose. In India, OPC and Alcohol are easily available so that one can procure these things very easily for poisoning. In some states like Gujrat and Bihar, consumption of alcohol is banned, which may prove to be good sign. Similar restriction should be warranted by the government to prevent easy access to insecticide like OPC.
First aid was given outside tertiary care hospital mainly by relatives of the patient before reaching to the hospital. People who did not receive first aid were probably brought to the hospital directly as they may have been geographically closer to the hospital and hence administered appropriate treatment earlier compared to others. Only 24% patients of Poisoning and 72% patients of snake bite received first aid. More social awareness in common public about role of first aid will contribute towards less hospital stay and more survival rate.
The median lag time in hospital arrival of poisoning and snake bite cases was 120 minutes and 90 minutes respectively. Factors mainly responsible for delay in lag time were due to inadequate facilities of transportation and referral from some other hospital. Significant difference (p<0.014) was observed between lag time and outcome. Median lag time in dead patients was 385 minutes as compared to 120 minutes in survived patients. Strategies to make transportation facilities available at primary level will minimize the lag time and will also improve outcome of the patient.
Out of total 99 hospitalized patients, 6% patients died due to poisoning. The findings of the present study are consistent with studies in developing and developed countries, which reveal a considerable increase in mortality and morbidity due to poisoning. [13,14] From Western countries, drugs like sedatives and analgesics have been reported as the most common substances abused, with mortality rates varying between 0.4% and 2.0%. [15-17]
The present study revealed that accidental poisoning (51.5%) and suicidal poisoning (47.5%) are the most common manner of acute poisoning. Alcohol intoxication was the major cause of accidental poisoning. More common intention of poisoning was suicide followed by accidental in studies done by Singh et al. [18] and Sharma et al. [19] An increase in the number of self-poisonings may be due to many factors such as more unemployment, urbanization, break up in family support system and economic instability. Suicide attempts among adults, especially in the age group of 21–40 years, could be due to lack of employment, break up in the family support system, failure of love affairs, an individual’s frustrations, inadequacy to cope with some immediate situation, impulsive behaviors, stress due to job and family, etc. Results of studies done by Singh et al. [20] and Lall et al. [20] reported that many deaths are due to organophosphate pesticides and occur in the young, economically active age group. Recent study done by Eddleston et al. [21] has shown that a high mortality is due to depression leading to suicide.
Also there is a trend for reduced duration of hospitalization, who received treatment outside tertiary care hospital, though difference was not statistically significant. It signifies the need and importance of early treatment in these cases. Study done by Mittal et al. [22] observed significant reduction in the duration of hospitalization in poisoning cases, who received outside treatment. In our study, we found that majority of the patients treated outside the hospital were AYUSH doctors (66%). There is a need to develop adequate strategies to improve the quality of treatment prior to referral to higher centre. It implies frequent hands on workshops for management of poisoning cases, training modules about handling of emergency cases and also availability of specific antidotes at primary level. Early access to treatment, increasing community health awareness and counseling can prove to be useful steps in this direction.
Early code blue activation revealed significantly better outcome. Code blue activation alerts doctors as well as paramedical staff to give early and rapid treatment to the patient with utmost care. Low PSS and lag time also revealed significantly better outcome. PSS mainly depends on exposure to poisoning (amount and duration), severity of poisoning and lag time before reaching to the hospital. In our study, it is revealed that Lag time does play very crucial role in determining outcome of the patient. Prolonged lag time mainly due to inadequate facilities of transportation and referral from some other hospital showed poor outcome. Delay in lag time and code blue activation prolongs the hospital stay thereby increasing cost of the treatment. More deaths had been observed in whom hospital stay was more than 3 days. This may be due to more PSS and prolonged lag time.
Results of the present study show that a higher mortality rate resulted due to organophosphate pesticides (5/6,83.3%). This may be because of easy availability, and uncontrolled sales and use of these agents. Among the total deaths reported, the majority (60%) of the patients were admitted in tertiary care hospital after 8 hrs of duration.
Despite the current controversial role of oximes in OPC poisonings and an insufficient evidence for their benefit-risk ratio, [23-25] Pralidoxime was used in the management of 62% OPC poisoning cases. In all patients of methanol poisoning, antidote ethanol was given for treatment. Prompt availability of antidotes is a matter of concern. Hence, strategies need to be implemented in order to improve the affordability and availability of antidotes, and improved evidence for their use in order to ensure a rational and cost-effective approach. [18]
Legislative measures to enforce the use of pesticides with low human toxicity and slow onset of action, reducing the bottle size and pesticide concentration might be helpful in decreasing the associated mortality burden. Also, steps can be taken to educate public about pesticide use and its harmful effects on body systems. [18] However, there is a continuous need to provide a more locally available and affordable hospital care at community level which includes hands on workshops and CMEs for management of poisoning.
Conclusion
OP compounds and alcoholic intoxication were the most common poisons, while sedatives were the common drugs encountered in drug overdose. Educational and awareness programs, establishment of poison information and surveillance centers and regulations on pesticides/drug availability will form one of the important strategies for the prevention of these emergencies. Better survival rate was observed in patients in whom Blue code was activated which reflect on good management of these emergencies at a tertiary care set-up. Reduction in lag time was reflected in better outcome, less hospital stay and thus cost of the treatment. Most of the patients received outside treatment by AYUSH doctors requiring frequent hands on workshops for management of poisoning cases, training modules about handling of emergency cases. Also there is a need of availability of specific antidotes at primary care level.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES
- Narayan Reddy KS, Murty OP. The Essentials of Forensic Medicine & Toxicology. Suguna Devi Publication. 31st edn, 2012; p: 464.
- Bertolote JM, Fleischmann A, Butchart A. Suicide, suicide attempts and pesticides: a major hidden public health problem. Bull World Health Organ 2006;84:260.
- Gunnell D, Eddleston M, Phillips MR. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 2007;7:357.
- Ramesha KN, Rao KB, Kumar GS. Pattern and outcome of acute poisoning cases in a tertiary care hospital in Karnataka, India. Indian J Crit Care Med 2009;13:152-5.
- Garg R, Aggarwal S, Singh H. Study of the relation of clinical and demographic factors with morbidity in a tertiary care teaching hospital in India. Int J Crit Illn Inj Sci 2013;3:12-7.
- Serkan EE, Ozge O, Oguz U, Arzu D, Akoglu H. World J Emerg Med 2014;5:20-3.
- Persson H, Sjöberg G, Haines J, Pronczuk de Garbino J. Poisoning Severity Score: Grading of acute poisoning. J Toxicology - Clinical Toxicology 1998;36:205-13.
- Cairans FJ, Koelmeyer TD, Smeeton WM. Deaths from drugs and poisons. NZ Med J 1982;96:1045-8.
- Nimal S, Laxman K. Pattern of acute poisoning in a medical unit in central Sri Lanka. Forensic Sci Int 1988;36:101-4.
- Tendon SK, Qureshi GU, Pandey DN, Aggarwal A. A profile of poisoning cases admitted in S.N. Medical College and Hospital, Agra. J Forensic Med Toxicol 1996;13:10-2.
- Tufekci IB, Curgunlu A, Sirin F. Characteristics of acute adult poisoning cases admitted to a university hospital in Istanbul. Hum Exp Toxicol 2004;23:347-51.
- Yamashita M, Matsuo H, Tanaka J. Analysis of 1000 consecutive cases of acute poisoning in the suburb of Tokyo leading to hospitalization. Vet Hum Toxicol. 1996;38:34-5.
- Singh S, Sharma BK, Wahi PL. Spectrum of acute poisoning in adults (10 years experience). J Assoc Physicians India. 1984;32:561-3.
- Tufekci IB, Curgunlu A, Sirin F. Characteristics of acute adult poisoning cases admitted to a university hospital in Istanbul. Hum Exp Toxicol 2004;23:347-51.
- Evans GJ. Deliberate self-poisoning in Oxford area. Br J Prev Soc Med 1967;21:97-107.
- Smith AJ. Self- poisoning with drugs: A worsening situation. Br Med J 1972;4:57-9.
- Rygnestad T. A comparative prospective study of self-poisoned patients in Trondheim, Norway between 1978 and 1987: Epidemiology and clinical data. Hum Toxicol. 1989;8:75-82.
- Singh S, Wig N, Chaudhary D, Sood N, Sharma B. Changing pattern of acute poisoning in adults: Experience of a large North West Indian hospital (1970-1989). J Assoc Physicians India. 1997;45:194-7.
- Sharma BR, Harish D, Sharma V, Vij K. Poisoning in Northern India: Changing trends, causes and prevention. Med Sci Law 2002;42:251-7.
- Lall SB, Peshin SS, Seth SS. Acute poisoning: A ten years retrospective hospital based study. Ann Natl Acad Med Sci 1994;30:35-4.
- Eddleston M, Singh S, Buckley N. Acute organophosphorus poisoning. Clin Evid 2003;9:1542-53.
- Mittal N, Nusrat S. A prospective observational study on different poisoning cases and their outcomes in a tertiary care hospital. SAGE Open Medicine 1: 2050312113504213.
- Peter JV, Moran JL, Graham P. Oxime therapy and outcomes in human organophosphate poisoning: an evaluation using meta-analytic techniques. Crit Care Med 2006;34:502-10.
- Buckley NA, Eddleston M, Szinicz L. Oximes for acute organophosphate pesticide poisoning. Cochrane Database Syst Rev 2005;1:CD005085.
- Eddleston M, Szinicz L, Eyer P. Oximes in acute organophosphorus pesticide poisoning: a systematic review of clinical trials. QJM 2002;95:275-283.